Principles of death certification
Demographic information
The Medical Certificate of Cause of Death (MCCD) collects a range of demographic information which is used for both legal and statistical purposes. It is important that the demographic information is recorded clearly and correctly as the accuracy of this information is vital to the quality of the national mortality dataset.
Complete all demographic details accurately including:
- name
- age
- sex/gender
- date of birth
- date of death
- place of death
- Indigenous status
Aboriginal and Torres Strait Islander information
The capacity of Commonwealth, State and Territory governments to report on issues such as the health status, service use and access to services by Aboriginal and Torres Strait Islander people is reliant on accurate identification. The Australian Bureau of Statistics (ABS) uses information from both the death registration statement and the MCCD to assist with understanding if a deceased person was of Aboriginal and/or Torres Strait Islander origin. The ABS mortality data is directly used to inform measures for Closing the Gap targets – accurate completion of this field is essential for robust information on the mortality of Aboriginal and Torres Strait Islander people.
It is not possible to determine whether the deceased is of Aboriginal or Torres Strait Islander origin without either asking someone who knew the deceased or checking administrative records. Assumptions should not be made based on appearance, family name or other personal characteristics.
If the Aboriginal and/or Torres Strait Islander origin of the deceased is unknown to you, one or more of the following processes should be undertaken:
- Ask the next of kin.
- Ask the broader family.
- Ask another person who knew the deceased well prior to their death.
- Review the medical record of the deceased (e.g. hospital admission, GP records).
Aboriginal or Torres Strait Islander status is used in a de-identified form to improve information on the health of Aboriginal or Torres Strait Islander and non-Indigenous Australians.
Legibility
Handwritten details can be difficult to distinguish and may lead to misinterpretation and error. Please avoid abbreviations and acronyms and if completing a handwritten certificate print clearly in block letters.
The following are examples of terms which are often difficult to distinguish:
- cardio/cerebro
- congenital/congestive
- coronary/cerebral
- empyema/emphysema
- hypotension/hypertension
- infection/infarction
- silicosis/scoliosis
- valvular/vascular
The standard Medical Certificate of Cause of Death
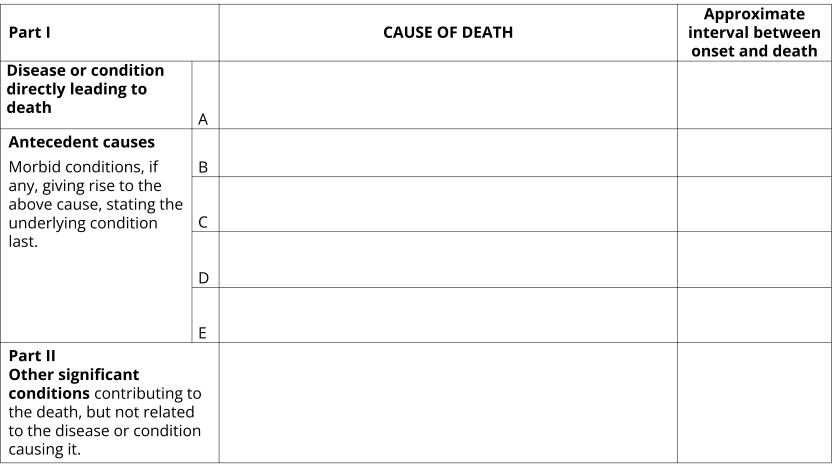
The Medical Certificate of Cause of Death (MCCD) is recommended by the World Health Organization for international use. This general format is used by all Australian states and territories, although some local variations will occur (e.g. an extra line, Part 1(e) appears on some forms). The extract below shows an example of the cause of death component of the certificate.
See Volume 2, Annex 7.1 of the ICD-10 for an example of the International MCCD.
Image
Description
Example of a blank Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
Completing the Medical Certificate of Cause of Death
As a Medical Practitioner you are required to lodge the MCCD with your state or territory Registry of Births, Deaths and Marriages. The quality of the statistics on causes of death depends on the quality of the information on the death certificate, which should be your best medical opinion as to the sequence of events leading to death.
When completing the MCCD enter the direct cause of death in Line 1(a) and the conditions which caused Line 1(a) in a temporal sequence, from top to bottom. The format is designed to work down the certificate – that is the condition in Line 1(a) should be caused by the condition in Line 1(b) which should be caused by the condition in Line 1(c), etc.
Part 1, Line 1(a), Disease or condition directly leading to death
Enter in Line 1(a) the direct cause of death i.e. the disease or complication which led directly to death.
When completing Line 1(a), keep in mind:
- There must always be an entry in Line 1(a) (do not leave it blank).
- This condition may be the only condition reported in Part 1 of the certificate only if it was not due to, or did not arise as a consequence of, any other disease or injury that occurred before the direct cause of death.
- The condition entered in Line 1(a) should have a shorter duration than any diseases mentioned in Line 1(b), Line 1(c), Line 1(d) or Line 1(e).
- If conditions such as cardiac arrest, respiratory failure or renal failure are entered in Line 1(a), always enter the underlying cause(s) of this condition in Line 1(b), Line 1(c), Line 1(d) and Line 1(e) to indicate the sequence of events leading to death.
- Commonly certified conditions in Line 1(a) include sepsis, metastases, pneumonia and traumatic injuries.
- Always use consecutive lines, never leave blank lines in the sequence.
- Do not use acronyms or abbreviations - clearly describe the disease or injury.
Part 1, Lines 1(b), 1(c), 1(d) and 1(e), Antecedent causes
If the direct cause of death in Line 1(a) was due to, or arose as a consequence of another disease, this disease should be entered in Line 1(b).
If the condition entered in Line 1(b) was itself due to another condition or disease this other condition should be reported in Line 1(c).
Similarly, a condition antecedent to that reported in Line 1(c) should be reported in Line 1(d). Enter any additional antecedent conditions in Line 1(d) and/or Line 1(e) if there is the option to do so. Note: Line 1(e) may appear on some forms. In this case, any antecedent conditions to that reported in Line 1(d) should be recorded in Line 1(e).
A condition should be regarded as being antecedent not only in an aetiological or pathological sense, but also where it is believed that this condition prepared the way for the direct cause by damage of tissues or impairment of function, even after a long interval.
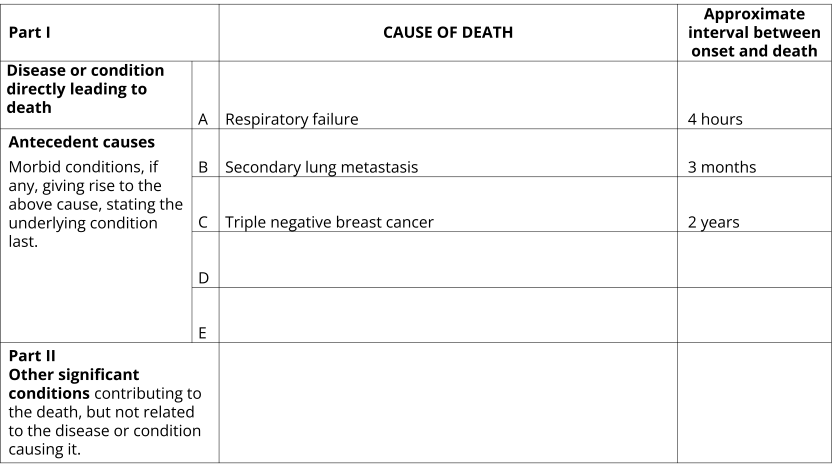
The following three examples show examples where Part 1 of the MCCD is accurately completed. Note that all three examples:
- Have a direct cause of death certified in Line 1(a).
- The antecedent causes conditions in Lines (b)-(e) are clearly listed in sequential order.
- Durations are included for each condition in Part 1.
- No acronyms or abbreviations are used.
Image
Description
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Respiratory failure. Approximate interval between onset and death: 4 hours
- Part 1(b): Secondary lung metastasis. Approximate interval between onset and death: 3 months
- Part 1(c): Triple negative breast cancer. Approximate interval between onset and death: 2 years
- Parts 1(d), 1(e) and 2: Blank. Approximate interval between onset and death: Blank
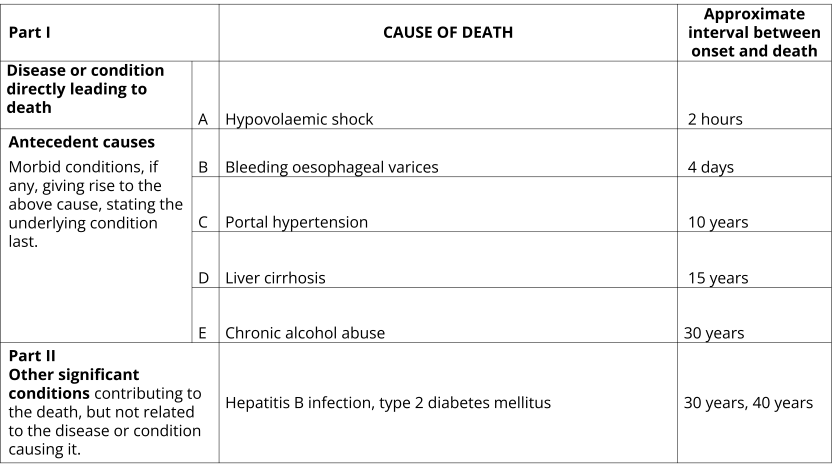
Image
Description
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line. The certificate is filled out as follows:
- Part 1(a): Hypovolaemic shock. Approximate interval between onset and death: 2 hours
- Part 1(b): Bleeding oesophageal varices. Approximate interval between onset and death: 4 days
- Part 1(c): Portal hypertension. Approximate interval between onset and death: 10 years
- Part 1(d): Liver cirrhosis. Approximate interval between onset and death: 15 years
- Part 1(e): Chronic alcohol abuse. Approximate interval between onset and death: 10 years
- Part 2: Hepatitis B infection, type 2 diabetes mellitus. Approximate interval between onset and death: 30 years, 40 years
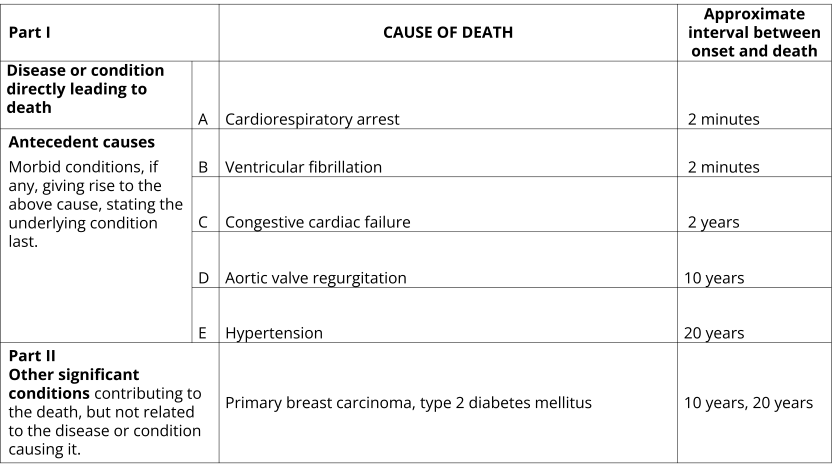
Image
Description
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Cardiorespiratory arrest. Approximate interval between onset and death: 2 minutes
- Part 1(b): Ventricular fibrillation. Approximate interval between onset and death: 2 minutes
- Part 1(c): Congestive cardiac failure. Approximate interval between onset and death: 2 years
- Part 1(d): Aortic valve regurgitation. Approximate interval between onset and death: 10 years
- Part 1(e): Hypertension. Approximate interval between onset and death: 20 years
- Part 2: Primary breast carcinoma, type 2 diabetes mellitus. Approximate interval between onset and death: 10 years, 20 years
Ideally, one condition per line should be certified. However, it is acknowledged that with an ageing population and more complex pathways to death there may be more than one cause that has led to the direct cause of death. Where two or more independent diseases are thought to have contributed equally to the fatal issue:
- They may be entered on the same line.
- Ensure the durations of the diseases are clearly stated for each disease.
The following two examples demonstrate how to accurately record two conditions on one line that have, in combination, led to death.
Image
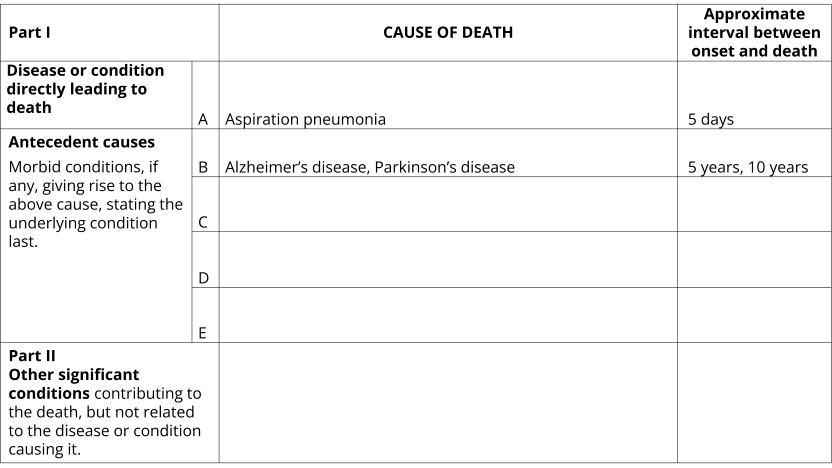
Description
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Aspiration pneumonia. Approximate interval between onset and death: 5 days
- Part 1(b): Alzheimer’s disease, Parkinson’s disease. Approximate interval between onset and death: 5 years, 10 years
- Parts 1(c), 1(d), 1(e) and 2: Blank. Approximate interval between onset and death: Blank
Image
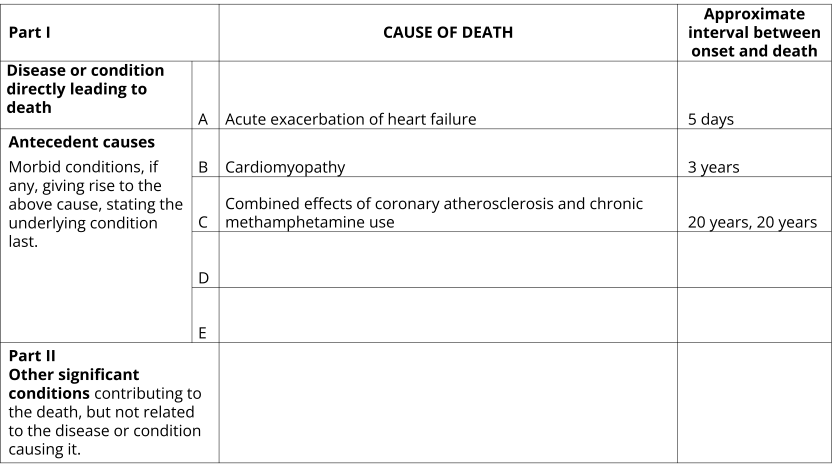
Description
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Acute exacerbation of heart failure. Approximate interval between onset and death: 5 days
- Part 1(b): Cardiomyopathy. Approximate interval between onset and death: 3 years
- Part 1(c): Combined effects of coronary atherosclerosis and chronic methamphetamine use. Approximate interval between onset and death: 20 years, 20 years
- Parts 1(d), 1(e) and 2: Blank. Approximate interval between onset and death: Blank
Approximate interval between onset and death
The duration between the onset of each condition entered on the certificate and the date of death should be entered in the column provided. The duration should represent when the condition is believed to have started (not necessarily when it was diagnosed).
Where the exact time or date of onset is not known, the best estimate should be made. Approximations such as 'more than 10 years' or 'approximately 6 months' are acceptable. A precise numeric measurement is not required if not known (e.g. 'years' is acceptable rather than '10 years'). If the duration of a condition cannot be ascertained writing 'unknown' is acceptable.
Durations may be entered using any of the following units of measurement:
- seconds
- minutes
- hours
- days
- weeks
- months
- years
- date of onset or diagnosis
The unit of time should be entered in each case and should generally be in chronological order. In a correctly completed certificate:
- The duration entered in Line 1(a) should not exceed the duration entered for the condition in Line 1(b), Line 1(c), Line 1(d) or Line 1(e).
- The duration for Line 1(b) should not exceed that for Line 1(c), Line 1(d) or Line 1(e).
Durations are used by ABS mortality coders to apply the most accurate code to a condition. For example, a stroke that occurred a few days before death will be coded to an acute cerebrovascular condition. A stroke that occurred over one year prior where sequelae effects have contributed to death will be coded a chronic cerebrovascular condition. Durations can also assist in understanding if a condition is congenital or acquired.
Image
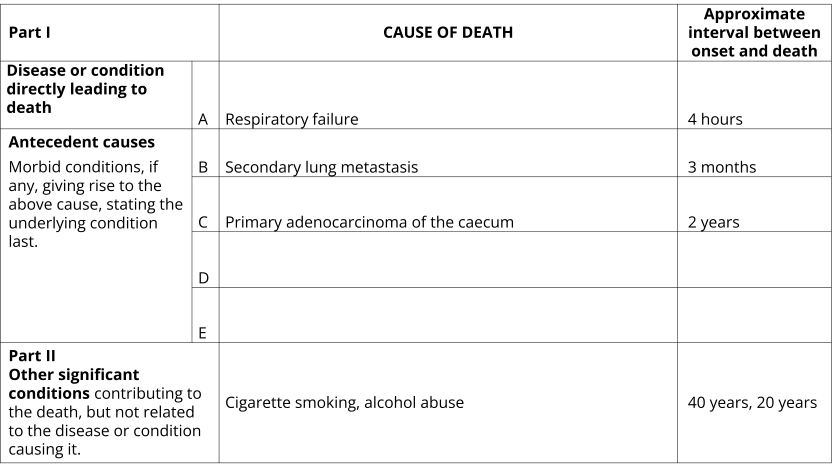
Description
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Example of a completed Medical Certificate of Cause of Death. The certificate is filled out as follows:
- Part 1(a): Respiratory failure. Approximate interval between onset and death: 4 hours
- Part 1(b): Secondary lung metastasis. Approximate interval between onset and death: 3 months
- Part 1(c): Primary adenocarcinoma of the caecum. Approximate interval between onset and death: 2 years
- Parts 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Cigarette smoking, alcohol abuse. Approximate interval between onset and death: 40 years, 20 years
Part 2, Other significant conditions
Certifiers must consider whether there were any other significant conditions which though not included in the sequence in Part 1, contributed to the fatal outcome.
If so, these conditions should be entered in Part 2. That is, diseases that did not directly cause the death but may have prevented the person from recovering from or overcoming the disease. This often includes chronic conditions (but is not limited to) such as diabetes, ischaemic heart disease, dementia or chronic obstructive pulmonary disease. Risk factors such as smoking, alcohol abuse, other drug use, obesity, etc. can also be certified in Part 2 if contributory to death and not in the sequence of events listed in Part 1.
Conditions in Part 2 of the MCCD should:
- Be present at the time of death.
- Have contributed to death.
- Not be included in the chain of events in Part 1 (these conditions should be in the correct part of the MCCD).
The following two examples show how conditions can be entered into Part 2 of the MCCD.
Image
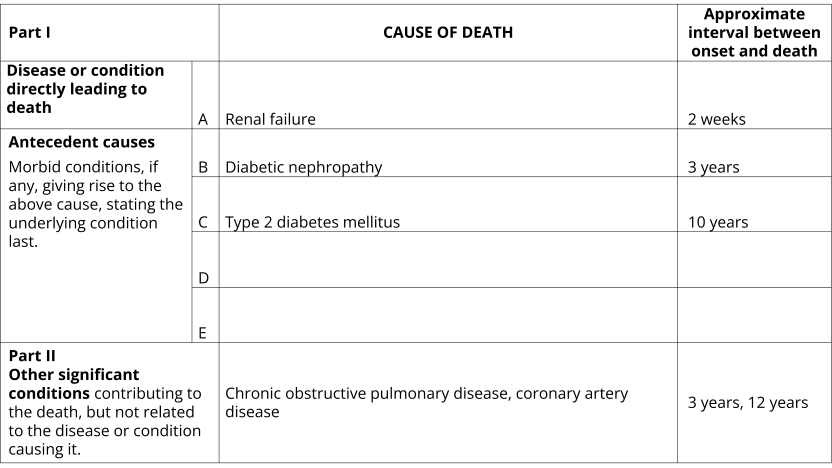
Description
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Renal failure. Approximate interval between onset and death: 2 weeks
- Part 1(b): Diabetic nephropathy. Approximate interval between onset and death: 3 years
- Part 1(c): Type 2 diabetes mellitus. Approximate interval between onset and death: 10 years
- Parts 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Chronic obstructive pulmonary disease, coronary artery disease. Approximate interval between onset and death: 3 years, 12 years
Image
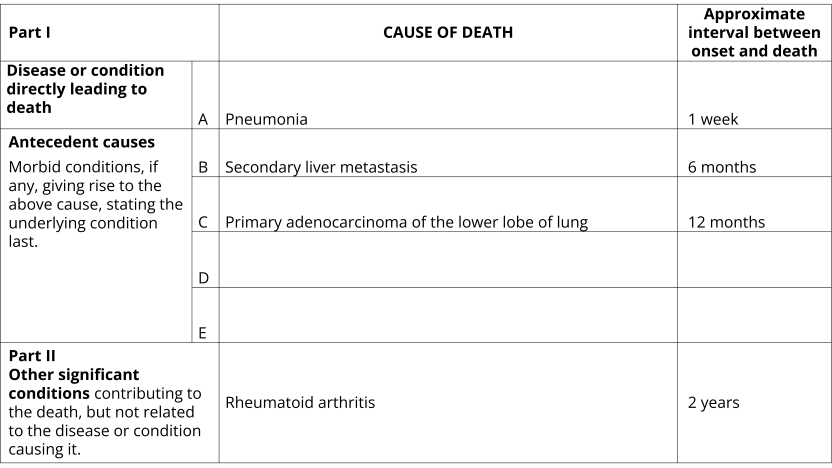
Description
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Pneumonia. Approximate interval between onset and death: 1 week
- Part 1(b): Secondary liver metastasis. Approximate interval between onset and death: 6 months
- Part 1(c): Primary adenocarcinoma of the lower lobe of lung. Approximate interval between onset and death: 12 months
- Parts 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Rheumatoid arthritis. Approximate interval between onset and death: 2 years
Surgical and medical procedures
In most jurisdictions, deaths related to health care must be reported to the Coroner for investigation. A health care related death is one where both the health care (or failure to provide health care) caused or contributed to death and the health care was not expected to cause death. Please refer to Deaths to be reported to the coroner.
Certification principles
- When entering a post operative complication, or a complication of a medical procedure, always include the condition for which the operation was performed and when the operation was performed.
- Only include a surgery or medical procedure if there is a resultant complication. The complication should also be certified and linked to the surgical or medical procedure.
- If a surgery or medical procedure caused a complication that contributed to death, these should be certified in the cause of death of death frame of the MCCD (either Part 1 or Part 2, depending on the circumstance). These can also be entered into the surgery/procedure box on the certificate if desired. However, if the surgery, medical procedure or complication are not included in the cause of death frame it is difficult at times to understand if this has been a causal factor in the death.
The following example shows how to accurately certify a death where a procedure has led to a complication.
Image
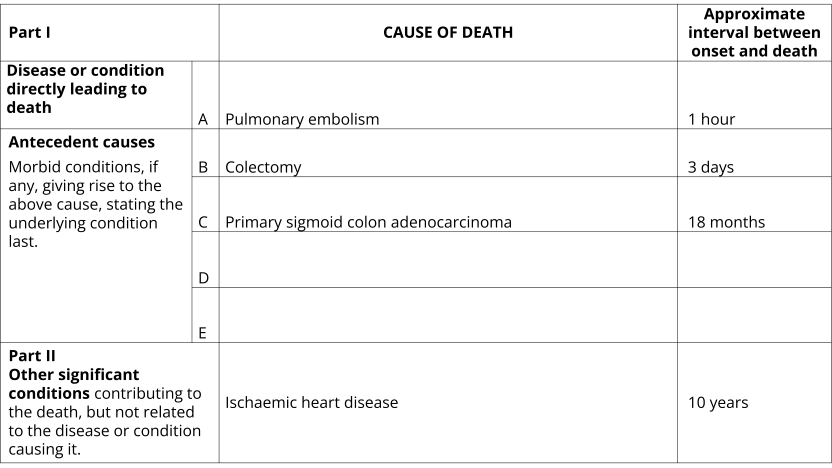
Description
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Pulmonary embolism. Approximate interval between onset and death: 1 hour
- Part 1(b): Colectomy. Approximate interval between onset and death: 3 days
- Part 1(c): Primary sigmoid colon adenocarcinoma. Approximate interval between onset and death: 18 months
- Parts 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Ischaemic heart disease. Approximate interval between onset and death: 10 years
Prophylactic medical treatments
The same principles for certifying surgical and medical procedures apply to certifying other medical treatments including those of a prophylactic nature. In recent years the ABS has received many queries on vaccines – namely whether the vaccine should be included on the MCCD and, if so, how should it be certified. Deaths due to vaccines are rare and it is important that correct procedures are followed. The below guidance can be applied to the certification of all prophylactic medical treatments if they have caused a complication contributing to or causing death.
- Check that the death should not be referred to the coroner. In the overwhelming majority of cases, these deaths would not be expected and should be referred for a coronial investigation.
- Ensure that a complication has occurred and that this complication has caused or contributed to death.
- Enter into Part 1 or Part 2 of the MCCD. Clearly certify the complication.
- Do not record any incidental treatments or measures in either the certificate frame or the surgery/procedure box.
The following example demonstrates the above principles. Note, that a complication that has contributed to death is clearly certified.
Image
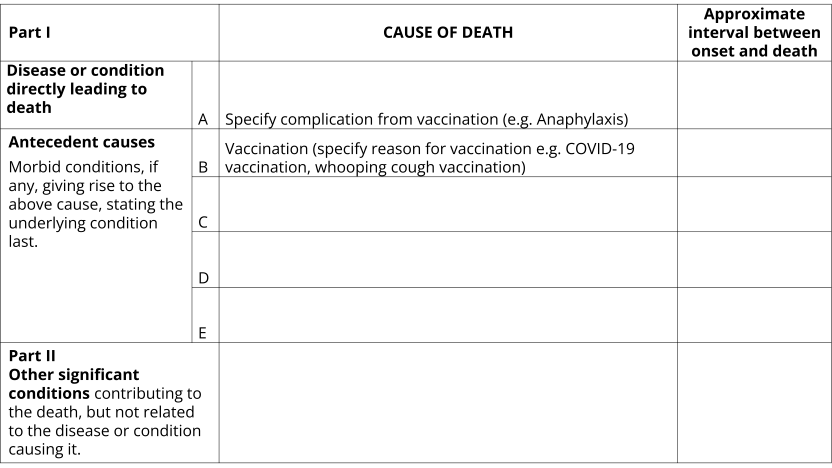
Description
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Specify complication from vaccination (e.g. Anaphylaxis). Approximate interval between onset and death: Blank
- Part 1(b): Vaccination (specify reason for vaccination e.g. COVID-19 vaccination, whooping cough vaccination). Approximate interval between onset and death: Blank
- Part 1(c): Primary sigmoid colon carcinoma. Approximate interval between onset and death: 18 months
- Parts 1(c), 1(d), 1(e) and 2: Blank. Approximate interval between onset and death: Blank
Causes requiring further specification
Where specificity is available, the conditions listed below require at least one of the qualifying terms to provide necessary details for identification of the underlying cause of death. Certifiers should be as specific as possible when certifying all conditions, not just those listed below. The list below shows examples of the types of qualifying terms that should be used to ensure sufficient specificity for identification of the underlying cause of death.
| Condition | Qualifying terms that should be used where applicable |
|---|---|
| Dementia | Alzheimer’s disease, vascular dementia, frontotemporal dementia, Lewy body dementia, dementia due to alcohol abuse, unspecified dementia |
| Diabetes | Type 1 diabetes mellitus, type 2 diabetes mellitus, gestational diabetes |
| Stroke | Cerebral infarction, cerebral haemorrhage, subarachnoid haemorrhage, subdural haemorrhage |
| Vascular disease | Generalised arteriosclerosis, coronary artery disease, cerebrovascular disease, peripheral vascular disease, coronary atherosclerosis |
| Valve disorder | Mitral stenosis, mitral insufficiency, mitral regurgitation, aortic stenosis, aortic insufficiency, aortic regurgitation |
| Endocarditis | Infective endocarditis, non-infective endocarditis |
| Chronic respiratory conditions | Emphysema, bronchiectasis, asthma, interstitial pulmonary fibrosis, chronic bronchitis, asbestosis |
| Kidney disease | Chronic kidney disease (enter stage if known), acute kidney disease, glomerulonephritis, acute tubular necrosis, hypertensive nephropathy |
Clinical diagnosis
The conditions listed on the MCCD should be the certifier's best medical opinion as to the as to the sequence of events leading to death. There may be times where a medical diagnosis is not possible. In these instances, it is acceptable to record a clinical diagnosis where this aligns with the certifier's best medical opinion. Where a clinical diagnosis is used, the following terms are acceptable: 'clinical diagnosis of,' 'likely,' or 'probable'. For example, the following terms are acceptable terminology:
- 'Lung mass - likely primary malignancy'.
- 'Clinical diagnosis of primary lung cancer'.
- 'Probable primary site of lung carcinoma'.
The following terms should not be written on the MCCD:
- 'Querying'. When the term 'querying' appears on the MCCD it is not clear if this is a clinical diagnosis or if laboratory tests are pending.
- 'Pending tests'. When this term appears it is not clear as to whether this condition should be included as a contributory cause of death.
- The use of '?' after a term. It is not clear if this is a clinical diagnosis or if laboratory tests are pending.
Ill-defined conditions
Ill-defined or non-specific conditions should not be reported alone on a certificate without another specified condition listed on the certificate. Ill-defined conditions should not be reported as the underlying cause of death. For example, cardiac arrest is considered an ill-defined condition. Cardiac arrest must not be reported alone or as the underlying cause of death without other further specified conditions indicating the cause or train of events which resulted in the cardiac arrest.
The list below highlights some examples of ill-defined conditions that should not be reported alone or as the underlying cause of death.
- Anuria
- Ascites
- Bradycardia
- Cardiac arrest
- Collapse
- Coma
- Constipation
- Cough
- Diarrhoea
- Dysphagia
- Fever
- Frailty
- Debility
- Haemoptysis
- Haemorrhage
- Headache
- Incontinence
- Infection
- Mass (intestinal, neck, head)
- Multi-organ failure
- Natural causes
- Nausea and vomiting
- Pain
- Paralysis
- Rash
- Respiratory failure
- Senility
- Syncope
- Tachycardia
Old age
Old age should be certified as the only cause on the MCCD in rare circumstances. The age of the deceased should not be the only factor used when determining a death is due to old age. Things to consider include:
- The medical history of the deceased.
- Any known chronic conditions or injuries which have contributed to death. These must be certified on the MCCD.
- An ongoing decline in the deceased’s health due to ageing should be noted.
- Where a very elderly person dies suddenly or unexpectedly, it may be insufficient to write 'old age'. Provided a clinician feels comfortable that the death is from natural causes and not notifiable to the coroner due to concerns for a specific reason, the clinician may consider what was the most likely cause of death. Where a clinician is still unsure, advice should be sought.
Natural causes
Deaths should not be certified with ‘natural causes’ as the only condition listed on the certificate. It is important that the specific natural causes being referenced are listed on the certificate.
For some coroner referred deaths, the cause of death may still be unknown after completion of forensic pathology where there is nothing to suggest that the death is due to anything other than natural causes. If the natural causes are known these should be certified (a clinical diagnosis here is acceptable, for example, that it is likely that death was due to the effects of ischaemic heart disease). If the specific diseases are not known or there is insufficient information for certification, the cause of death should say 'unascertained natural causes'.
Conditions unlikely to cause death
Some conditions are considered unlikely to cause death. These conditions should not be certified on the MCCD alone and in most circumstances should not be reported on the lowest used line of the MCCD as the underlying cause of death. The only exceptions to this are rare circumstances where the condition has caused severe outcomes initiating a train of events leading to death or there has been an adverse outcome from a procedure/medication performed for a condition unlikely to cause death.
See Volume 2, Annex 7.4 of the ICD-10 for a list of trivial conditions unlikely to cause death that should not be used as the underlying cause.
The following example shows how a condition that may be considered unlikely to cause death may be certified.
Image
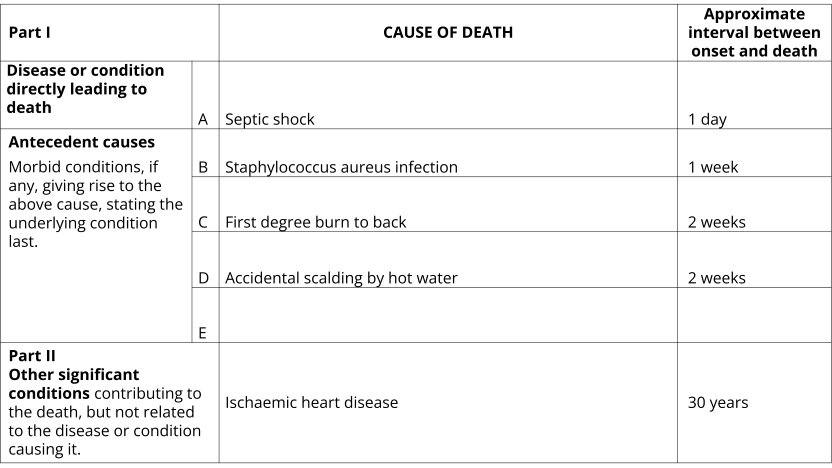
Description
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Septic shock. Approximate interval between onset and death: 1 day
- Part 1(b): Staphylococcus aureus infection. Approximate interval between onset and death: 1 week
- Part 1(c): First degree burn to back. Approximate interval between onset and death: 2 weeks
- Part 1(d): Accidental scalding by hot water. Approximate interval between onset and death: 2 weeks
- Parts 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Ischaemic heart disease. Approximate interval between onset and death: 30 years