Cause of death certification guide
A guide to assist doctors to accurately complete the Medical Certificate of Cause of Death in Australia.
Purpose of this guide
The purpose of this guide is to assist certifiers in understanding how to accurately complete the Medical Certificate of Cause of Death (MCCD) to increase the quality of the national mortality dataset, and expedite the processing of death certificates and aggregation of cause of death data. Information and examples for the most common issues encountered are identified later in this guide.
There is also a separate section for guidance on how to complete a Medical Certificate of Cause of Perinatal Death (MCCPD).
This guide provides advice on the completion of the MCCD and MCCPD only. It does not extend to other reporting requirements such as notifiable conditions or adverse effects reporting. Please seek advice from relevant health authorities for such requirements.
The information provided is not intended as a guide to the legal requirements of death certification, notification of death or of cases that require reporting to the coroner. These requirements differ between jurisdictions. For advice on your legal obligations please contact your state or territory Coroner's Office.
Importance of cause of death information
The MCCD completed by medical practitioners is the major source of Australia's mortality statistics. The use of mortality statistics for demographic and health purposes supports understanding of Australian society now and in the future. These statistics guide the formulation and monitoring of health and lifestyle policies and impact on the funding of medical and health research. Accurate cause of death information is also important to family members to understand what caused a loved one’s death and to be aware of conditions that may occur in other family members.
After registration of the death:
- The Registrar of Births, Deaths and Marriages in each state or territory provides the information on the MCCD to the Australian Bureau of Statistics (ABS).
- ABS staff code the conditions listed on the MCCD according to the International Statistical Classification of Diseases and Related Health Problems (ICD). The 10th revision of the ICD is currently used by the ABS (ICD-10). The ICD is produced by the World Health Organization, and is the international standard diagnostic classification used to classify diseases and other health problems recorded on many types of health and vital records including death certificates and hospital records.
- An ICD-10 code is assigned to every condition on the death certificate. In a large proportion of deaths, a sequence of morbid events will have led to death. From the standpoint of prevention, the objective is to break the sequence as early as possible, hence information on every condition is required.
- Coding rules are applied to assign an underlying cause of death.
- The ABS compiles the national mortality dataset utilising the coded data from the MCCD.
- Causes of death for doctor certified deaths are processed monthly and are released in the Provisional Mortality Statistics publication. The collective causes of death dataset including both doctor and coroner certified deaths are released annually in Causes of Death, Australia. This publication includes summaries of the dataset. Special tabulations are also available upon request from the ABS.
- The data produced by the ABS is used by government bodies, researchers, clinicians, educational institutions and many other organisations.
Assistance and contact information
This guide is provided to assist medical practitioners to report accurate information to support coding of cause of death. If you have any questions or would like further information, please contact the Australian Bureau of Statistics on phone toll free: 1800 620 963.
The ABS is unable to provide blank medical certificates. Please contact the Registrar of Births, Deaths and Marriages in your state or territory (see contact details below).
Blank Medical Certificates of Cause of Death
The ABS is unable to provide blank medical certificates. Blank MCCDs for completion may be requested from the Registrar of Births, Deaths and Marriages in your state or territory.
| Jurisdiction | Phone number | Website |
|---|---|---|
| New South Wales Registry of Birth, Deaths & Marriages | 13 77 88 | https://www.service.nsw.gov.au/transaction/order-a-medical-certificate-cause-of-death-mccd-form |
| Victoria Registry of Births, Deaths & Marriages | 1300 369 367 | https://www.bdm.vic.gov.au/medical-practitioners |
| Queensland Registry of Births, Deaths & Marriages | 13 74 68 | https://www.qld.gov.au/law/births-deaths-marriages-and-divorces/online-service-providers/medical-practitioners |
| South Australia Births, Deaths & Marriages | 131 882 | https://www.sa.gov.au/topics/family-and-community/births-deaths-and-marriages/when-someone-dies/doctors-and-funeral-directors/doctors |
| Western Australia Registry of Births, Deaths & Marriages | 1300 305 021 | Email: bdm@justice.wa.gov.au |
| Tasmania Births, Deaths & Marriages | 1300 135 513 | https://www.justice.tas.gov.au/bdm/register-death |
| Northern Territory Registry of Births, Deaths, and Marriages | 08 8999 6119 | https://nt.gov.au/law/bdm/births-deaths-and-marriages-office-contacts |
| Australian Capital Territory Registrar-General's Office | 13 22 81 | Email: bdm@act.gov.au |
| Norfolk Island Register of Births, Deaths and Marriages | +6723 23691 | Email: registrar@bdm.gov.nf |
Deaths to be reported to the coroner
What constitutes a 'reportable death' varies by jurisdiction. In general, a death must be reported to a coroner in the following instances:
- where the person died unexpectedly, and the cause of death is unknown
- where the death resulted, directly or indirectly, from an accident or injury, even if there has been a prolonged interval between the incident and death
- where the person died in a violent or unnatural manner
- where the person died during, or as a result of, a medical procedure
- where the person was held in care or in custody immediately before they died (noting that ‘in care’ excludes facilities such as residential aged care)
- where a doctor has been unable to sign a death certificate giving the cause of death
- where the identity of the person who has died is not known.
If you are unsure whether a death should be reported to the coroner, please contact the Coroner's Office in your state or territory for further advice.
Advice on reportable deaths
If you are in any doubt as to whether a death should be reported to the coroner, please contact the Coroner's Office in your state or territory for further advice.
| Jurisdiction | Phone number |
|---|---|
| Coroners Court of New South Wales | 02 8584 7777 |
| Coroners Court of Victoria | 1300 309 519 |
| Coroners Court of Queensland | 07 3738 7050 |
| Coroners Court of South Australia | 08 8204 0600 |
| Coroners Court of Western Australia | 08 9425 2900 |
| Coroners Court of Tasmania | 03 6165 7134 |
| Northern Territory Coroner's Office | 08 8999 7770 |
| Coroners Court of Australian Capital Territory | 02 6207 1754 |
| Coroners Court of Norfolk Island | +6723 23691 |
Acknowledgements
The ABS would like to acknowledge the assistance provided by Dr Mitchell Shaw, Dr Amy Weber and Dr Ian Holme of Clinical Excellence Queensland.
Principles of death certification
Demographic information
The Medical Certificate of Cause of Death (MCCD) collects a range of demographic information which is used for both legal and statistical purposes. It is important that the demographic information is recorded clearly and correctly as the accuracy of this information is vital to the quality of the national mortality dataset.
Complete all demographic details accurately including:
- name
- age
- sex/gender
- date of birth
- date of death
- place of death
- Indigenous status
Aboriginal and Torres Strait Islander information
The capacity of Commonwealth, State and Territory governments to report on issues such as the health status, service use and access to services by Aboriginal and Torres Strait Islander people is reliant on accurate identification. The Australian Bureau of Statistics (ABS) uses information from both the death registration statement and the MCCD to assist with understanding if a deceased person was of Aboriginal and/or Torres Strait Islander origin. The ABS mortality data is directly used to inform measures for Closing the Gap targets – accurate completion of this field is essential for robust information on the mortality of Aboriginal and Torres Strait Islander people.
It is not possible to determine whether the deceased is of Aboriginal or Torres Strait Islander origin without either asking someone who knew the deceased or checking administrative records. Assumptions should not be made based on appearance, family name or other personal characteristics.
If the Aboriginal and/or Torres Strait Islander origin of the deceased is unknown to you, one or more of the following processes should be undertaken:
- Ask the next of kin.
- Ask the broader family.
- Ask another person who knew the deceased well prior to their death.
- Review the medical record of the deceased (e.g. hospital admission, GP records).
Aboriginal or Torres Strait Islander status is used in a de-identified form to improve information on the health of Aboriginal or Torres Strait Islander and non-Indigenous Australians.
Legibility
Handwritten details can be difficult to distinguish and may lead to misinterpretation and error. Please avoid abbreviations and acronyms and if completing a handwritten certificate print clearly in block letters.
The following are examples of terms which are often difficult to distinguish:
- cardio/cerebro
- congenital/congestive
- coronary/cerebral
- empyema/emphysema
- hypotension/hypertension
- infection/infarction
- silicosis/scoliosis
- valvular/vascular
The standard Medical Certificate of Cause of Death
The Medical Certificate of Cause of Death (MCCD) is recommended by the World Health Organization for international use. This general format is used by all Australian states and territories, although some local variations will occur (e.g. an extra line, Part 1(e) appears on some forms). The extract below shows an example of the cause of death component of the certificate.
See Volume 2, Annex 7.1 of the ICD-10 for an example of the International MCCD.
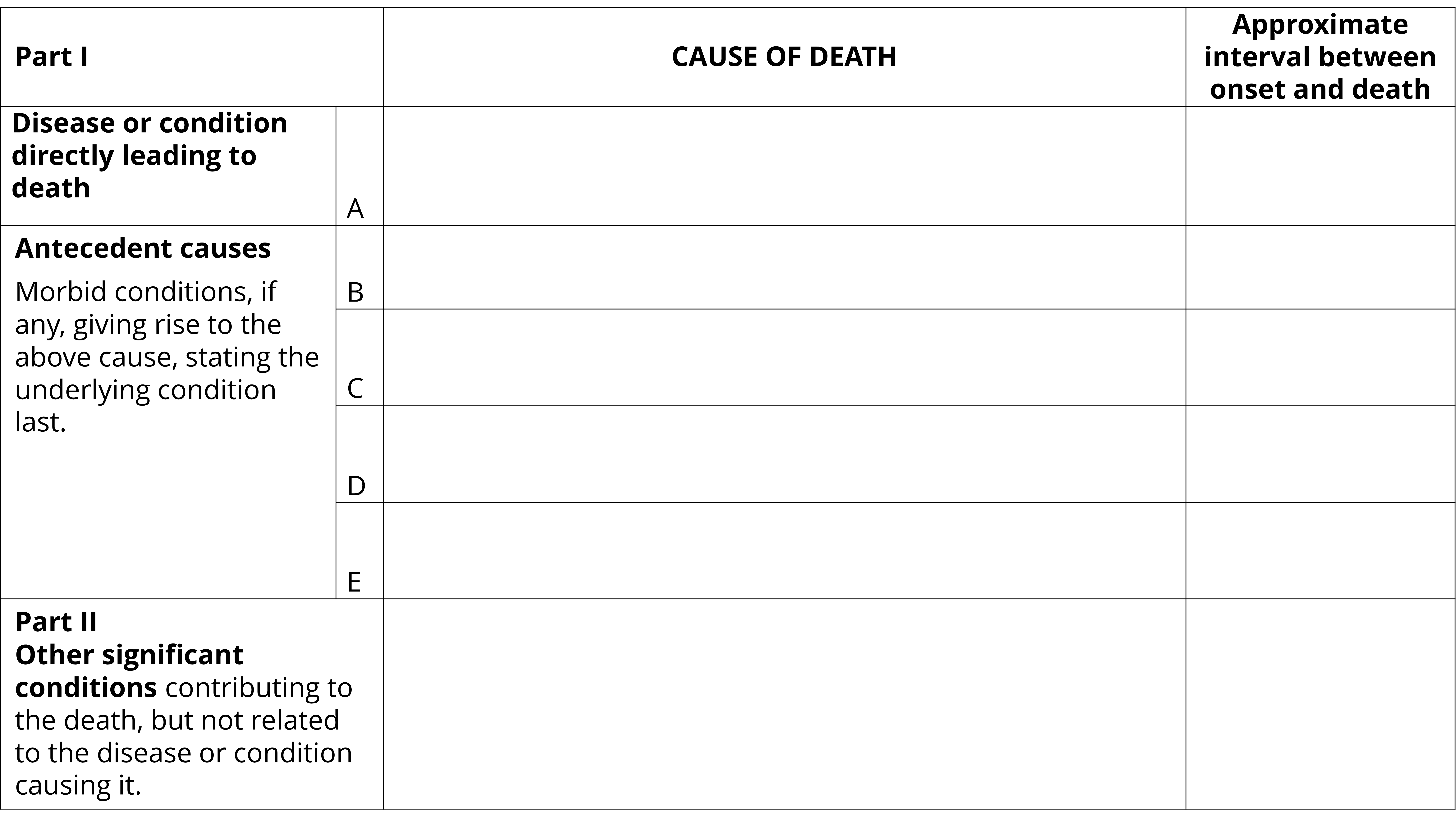
Example of a blank Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
Completing the Medical Certificate of Cause of Death
As a Medical Practitioner you are required to lodge the MCCD with your state or territory Registry of Births, Deaths and Marriages. The quality of the statistics on causes of death depends on the quality of the information on the death certificate, which should be your best medical opinion as to the sequence of events leading to death.
When completing the MCCD enter the direct cause of death in Line 1(a) and the conditions which caused Line 1(a) in a temporal sequence, from top to bottom. The format is designed to work down the certificate – that is the condition in Line 1(a) should be caused by the condition in Line 1(b) which should be caused by the condition in Line 1(c), etc.
Part 1, Line 1(a), Disease or condition directly leading to death
Enter in Line 1(a) the direct cause of death i.e. the disease or complication which led directly to death.
When completing Line 1(a), keep in mind:
- There must always be an entry in Line 1(a) (do not leave it blank).
- This condition may be the only condition reported in Part 1 of the certificate only if it was not due to, or did not arise as a consequence of, any other disease or injury that occurred before the direct cause of death.
- The condition entered in Line 1(a) should have a shorter duration than any diseases mentioned in Line 1(b), Line 1(c), Line 1(d) or Line 1(e).
- If conditions such as cardiac arrest, respiratory failure or renal failure are entered in Line 1(a), always enter the underlying cause(s) of this condition in Line 1(b), Line 1(c), Line 1(d) and Line 1(e) to indicate the sequence of events leading to death.
- Commonly certified conditions in Line 1(a) include sepsis, metastases, pneumonia and traumatic injuries.
- Always use consecutive lines, never leave blank lines in the sequence.
- Do not use acronyms or abbreviations - clearly describe the disease or injury.
Part 1, Lines 1(b), 1(c), 1(d) and 1(e), Antecedent causes
If the direct cause of death in Line 1(a) was due to, or arose as a consequence of another disease, this disease should be entered in Line 1(b).
If the condition entered in Line 1(b) was itself due to another condition or disease this other condition should be reported in Line 1(c).
Similarly, a condition antecedent to that reported in Line 1(c) should be reported in Line 1(d). Enter any additional antecedent conditions in Line 1(d) and/or Line 1(e) if there is the option to do so. Note: Line 1(e) may appear on some forms. In this case, any antecedent conditions to that reported in Line 1(d) should be recorded in Line 1(e).
A condition should be regarded as being antecedent not only in an aetiological or pathological sense, but also where it is believed that this condition prepared the way for the direct cause by damage of tissues or impairment of function, even after a long interval.
The following three examples show examples where Part 1 of the MCCD is accurately completed. Note that all three examples:
- Have a direct cause of death certified in Line 1(a).
- The antecedent causes conditions in Lines (b)-(e) are clearly listed in sequential order.
- Durations are included for each condition in Part 1.
- No acronyms or abbreviations are used.
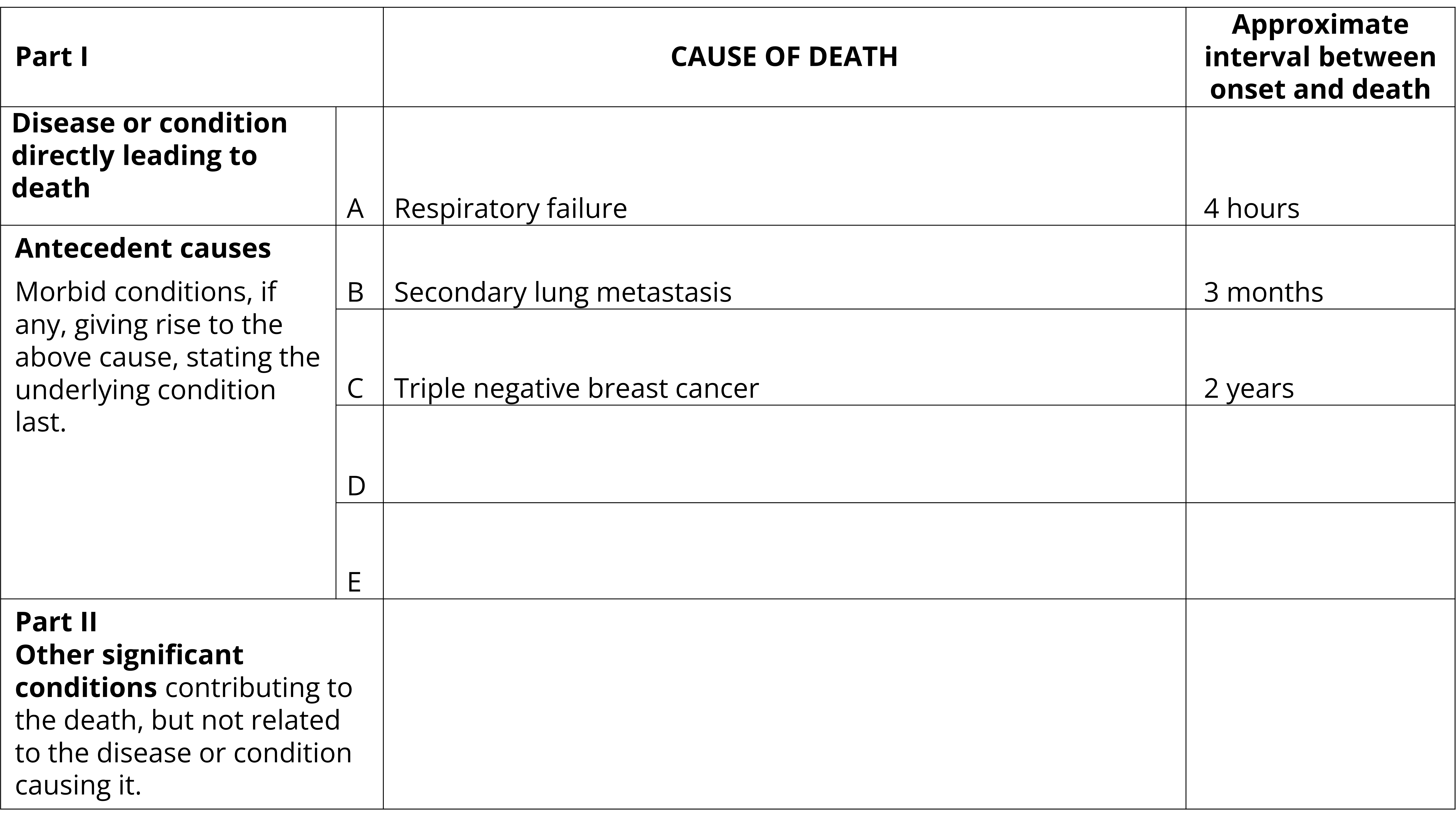
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Respiratory failure. Approximate interval between onset and death: 4 hours
- Part 1(b): Secondary lung metastasis. Approximate interval between onset and death: 3 months
- Part 1(c): Triple negative breast cancer. Approximate interval between onset and death: 2 years
- Parts 1(d), 1(e) and 2: Blank. Approximate interval between onset and death: Blank
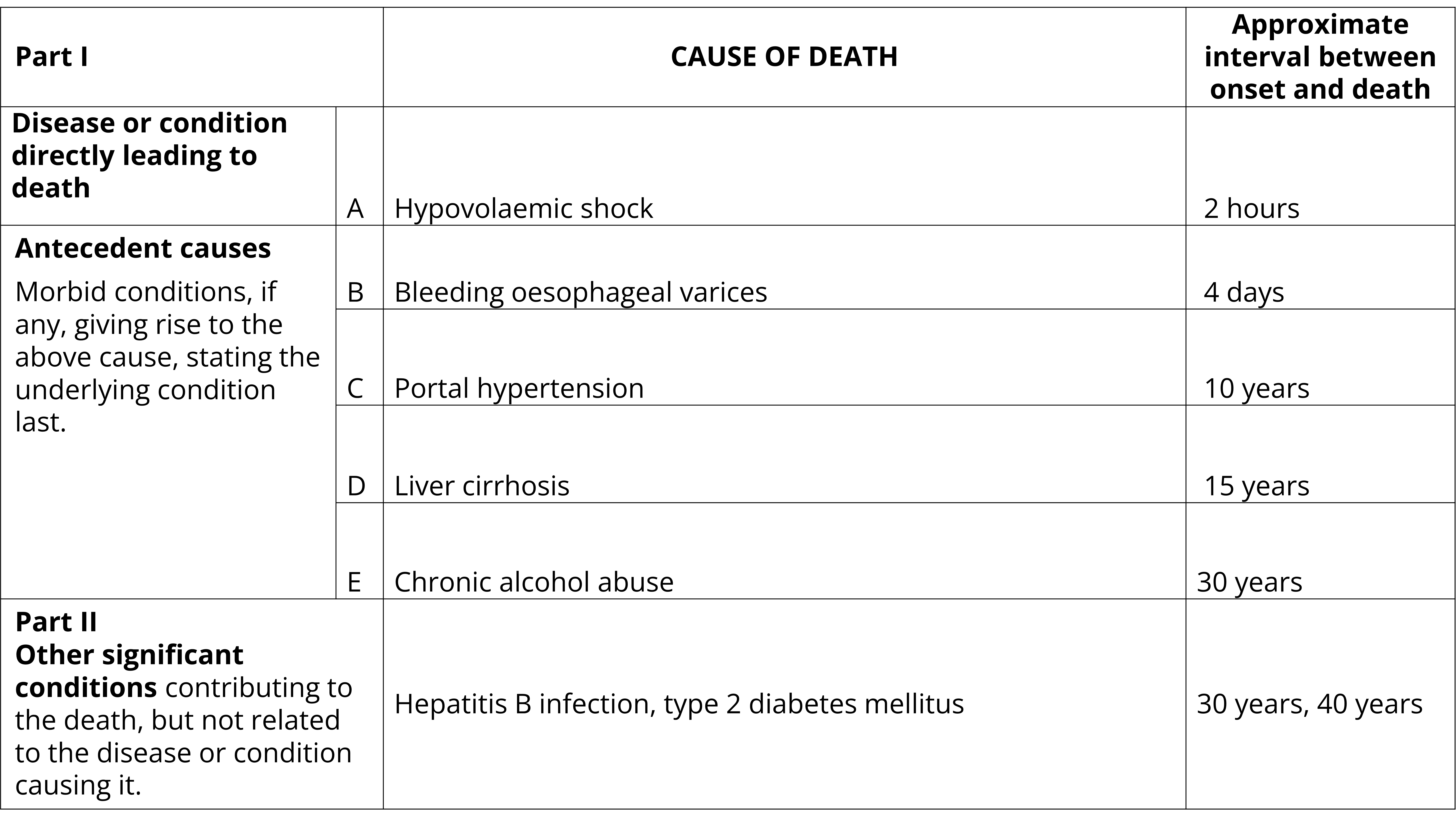
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line. The certificate is filled out as follows:
- Part 1(a): Hypovolaemic shock. Approximate interval between onset and death: 2 hours
- Part 1(b): Bleeding oesophageal varices. Approximate interval between onset and death: 4 days
- Part 1(c): Portal hypertension. Approximate interval between onset and death: 10 years
- Part 1(d): Liver cirrhosis. Approximate interval between onset and death: 15 years
- Part 1(e): Chronic alcohol abuse. Approximate interval between onset and death: 10 years
- Part 2: Hepatitis B infection, type 2 diabetes mellitus. Approximate interval between onset and death: 30 years, 40 years
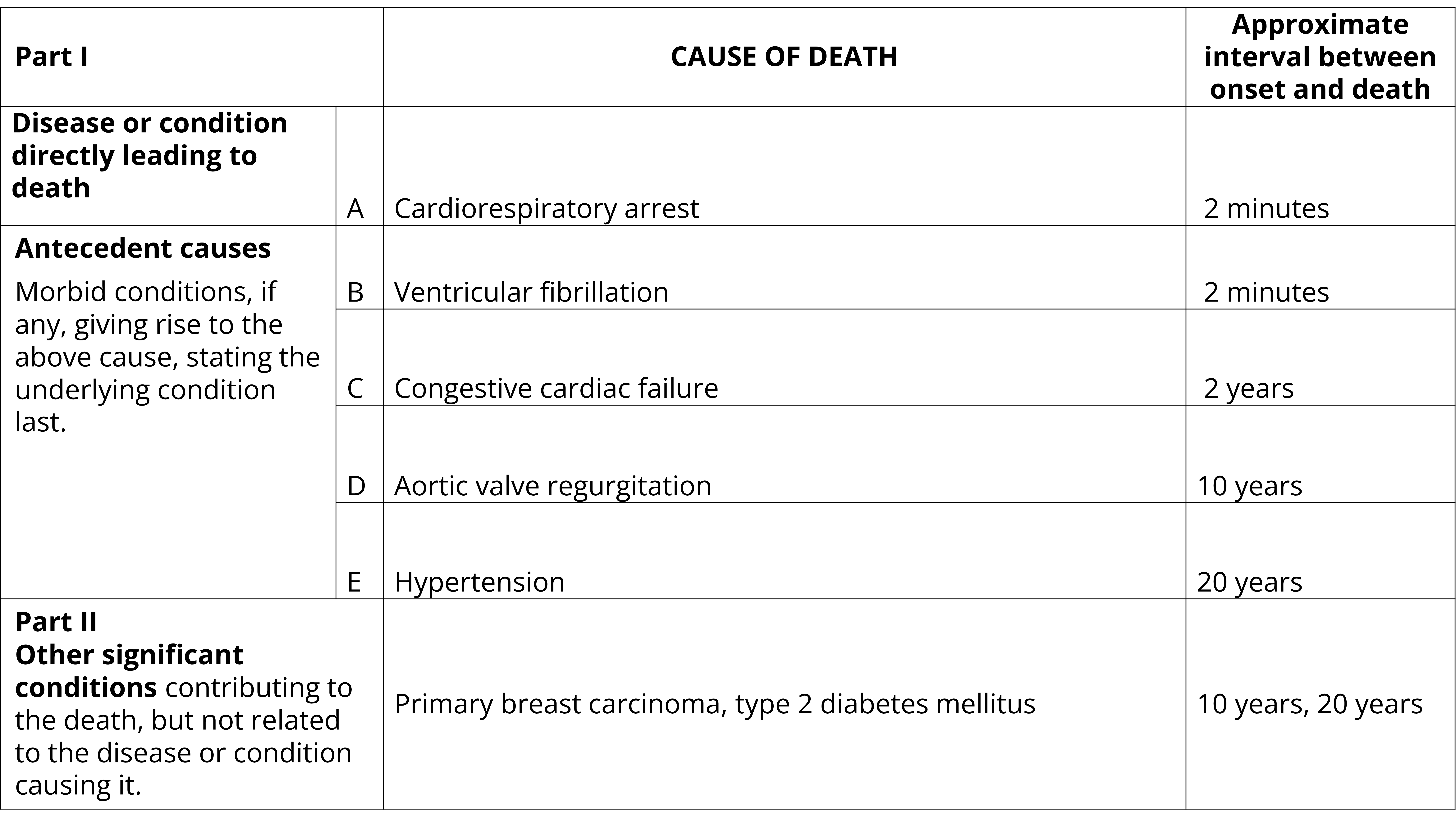
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Cardiorespiratory arrest. Approximate interval between onset and death: 2 minutes
- Part 1(b): Ventricular fibrillation. Approximate interval between onset and death: 2 minutes
- Part 1(c): Congestive cardiac failure. Approximate interval between onset and death: 2 years
- Part 1(d): Aortic valve regurgitation. Approximate interval between onset and death: 10 years
- Part 1(e): Hypertension. Approximate interval between onset and death: 20 years
- Part 2: Primary breast carcinoma, type 2 diabetes mellitus. Approximate interval between onset and death: 10 years, 20 years
Ideally, one condition per line should be certified. However, it is acknowledged that with an ageing population and more complex pathways to death there may be more than one cause that has led to the direct cause of death. Where two or more independent diseases are thought to have contributed equally to the fatal issue:
- They may be entered on the same line.
- Ensure the durations of the diseases are clearly stated for each disease.
The following two examples demonstrate how to accurately record two conditions on one line that have, in combination, led to death.
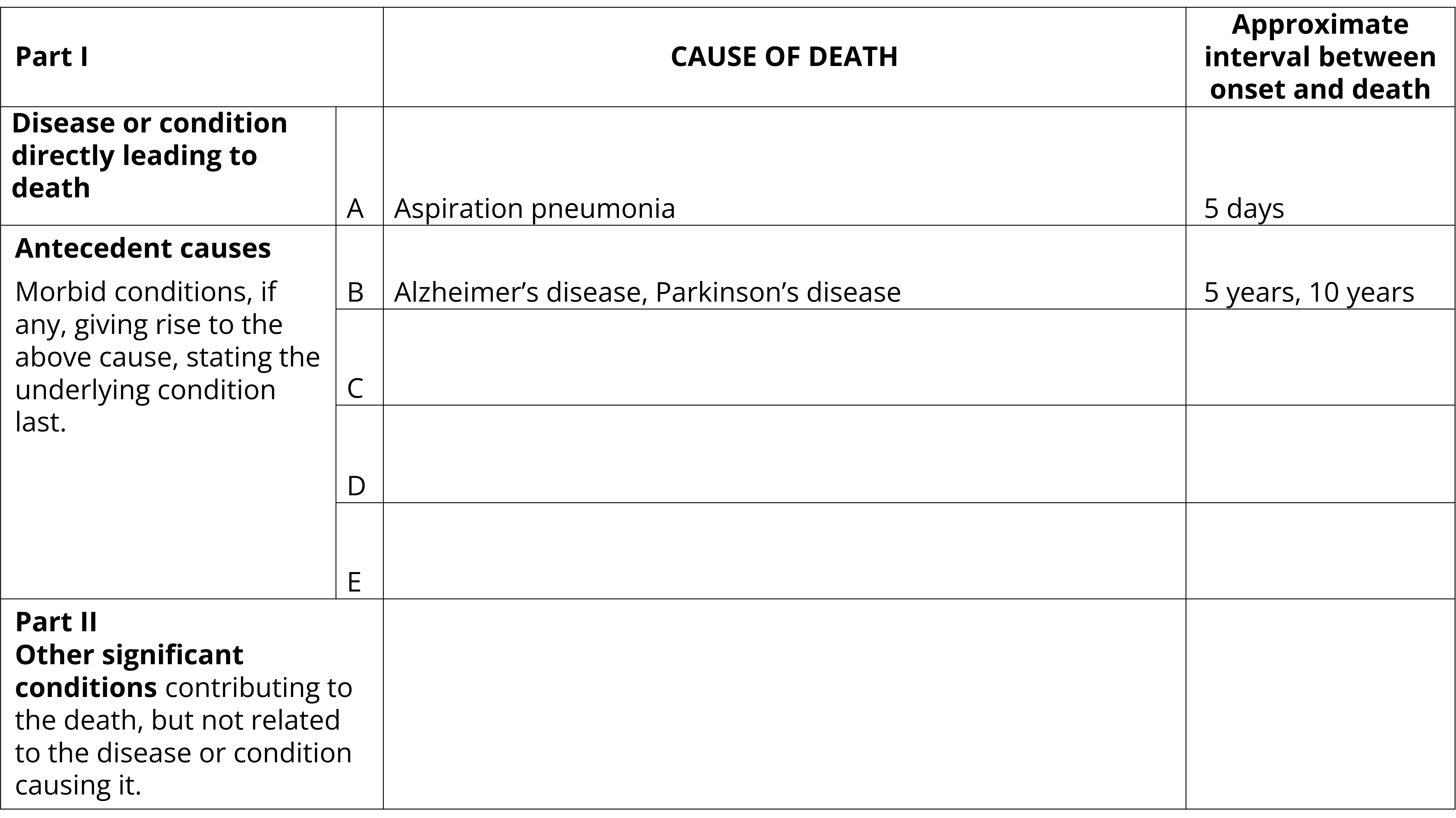
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Aspiration pneumonia. Approximate interval between onset and death: 5 days
- Part 1(b): Alzheimer’s disease, Parkinson’s disease. Approximate interval between onset and death: 5 years, 10 years
- Parts 1(c), 1(d), 1(e) and 2: Blank. Approximate interval between onset and death: Blank
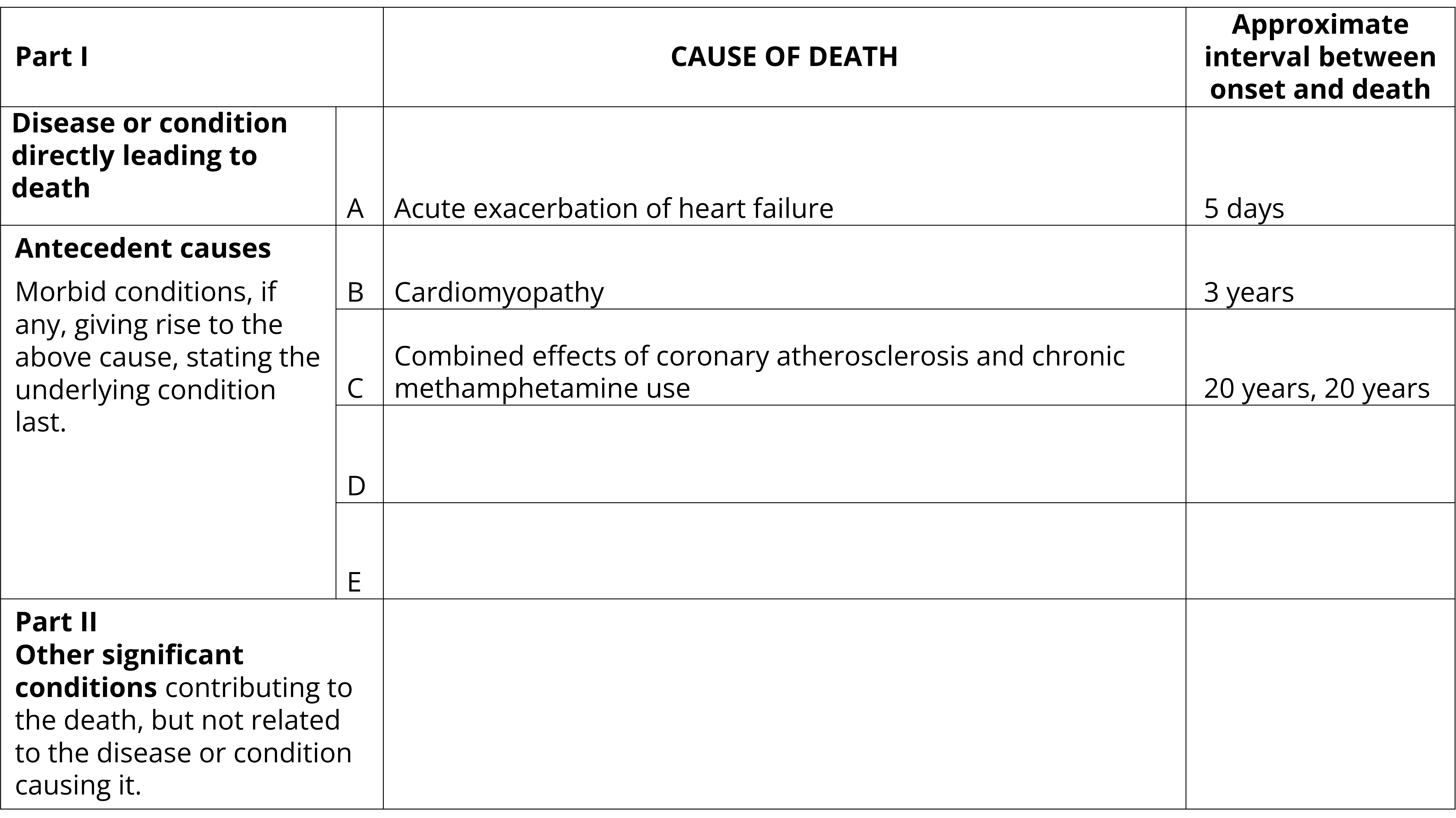
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Acute exacerbation of heart failure. Approximate interval between onset and death: 5 days
- Part 1(b): Cardiomyopathy. Approximate interval between onset and death: 3 years
- Part 1(c): Combined effects of coronary atherosclerosis and chronic methamphetamine use. Approximate interval between onset and death: 20 years, 20 years
- Parts 1(d), 1(e) and 2: Blank. Approximate interval between onset and death: Blank
Approximate interval between onset and death
The duration between the onset of each condition entered on the certificate and the date of death should be entered in the column provided. The duration should represent when the condition is believed to have started (not necessarily when it was diagnosed).
Where the exact time or date of onset is not known, the best estimate should be made. Approximations such as 'more than 10 years' or 'approximately 6 months' are acceptable. A precise numeric measurement is not required if not known (e.g. 'years' is acceptable rather than '10 years'). If the duration of a condition cannot be ascertained writing 'unknown' is acceptable.
Durations may be entered using any of the following units of measurement:
- seconds
- minutes
- hours
- days
- weeks
- months
- years
- date of onset or diagnosis
The unit of time should be entered in each case and should generally be in chronological order. In a correctly completed certificate:
- The duration entered in Line 1(a) should not exceed the duration entered for the condition in Line 1(b), Line 1(c), Line 1(d) or Line 1(e).
- The duration for Line 1(b) should not exceed that for Line 1(c), Line 1(d) or Line 1(e).
Durations are used by ABS mortality coders to apply the most accurate code to a condition. For example, a stroke that occurred a few days before death will be coded to an acute cerebrovascular condition. A stroke that occurred over one year prior where sequelae effects have contributed to death will be coded a chronic cerebrovascular condition. Durations can also assist in understanding if a condition is congenital or acquired.
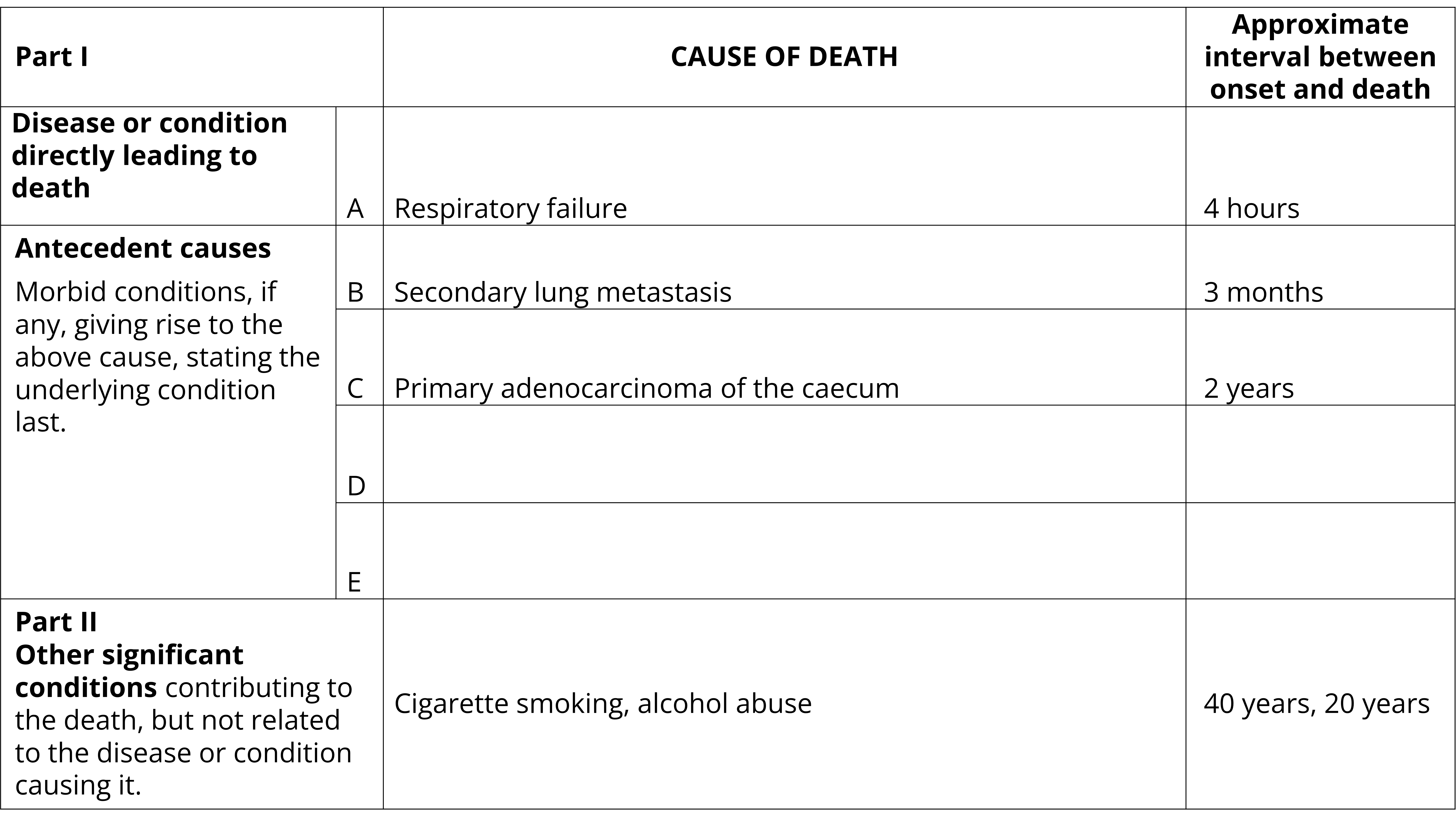
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Example of a completed Medical Certificate of Cause of Death. The certificate is filled out as follows:
- Part 1(a): Respiratory failure. Approximate interval between onset and death: 4 hours
- Part 1(b): Secondary lung metastasis. Approximate interval between onset and death: 3 months
- Part 1(c): Primary adenocarcinoma of the caecum. Approximate interval between onset and death: 2 years
- Parts 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Cigarette smoking, alcohol abuse. Approximate interval between onset and death: 40 years, 20 years
Part 2, Other significant conditions
Certifiers must consider whether there were any other significant conditions which though not included in the sequence in Part 1, contributed to the fatal outcome.
If so, these conditions should be entered in Part 2. That is, diseases that did not directly cause the death but may have prevented the person from recovering from or overcoming the disease. This often includes chronic conditions (but is not limited to) such as diabetes, ischaemic heart disease, dementia or chronic obstructive pulmonary disease. Risk factors such as smoking, alcohol abuse, other drug use, obesity, etc. can also be certified in Part 2 if contributory to death and not in the sequence of events listed in Part 1.
Conditions in Part 2 of the MCCD should:
- Be present at the time of death.
- Have contributed to death.
- Not be included in the chain of events in Part 1 (these conditions should be in the correct part of the MCCD).
The following two examples show how conditions can be entered into Part 2 of the MCCD.
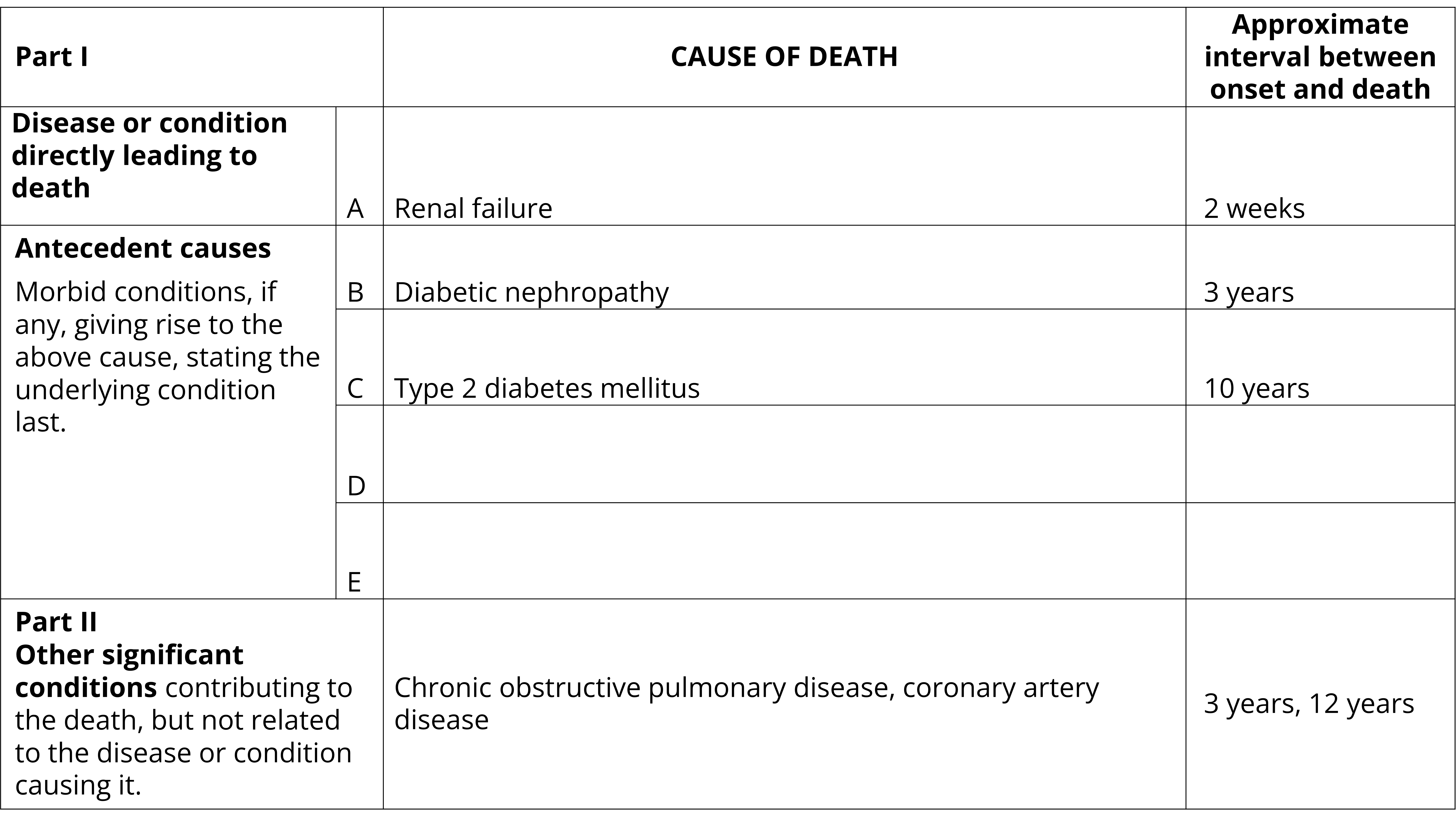
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Renal failure. Approximate interval between onset and death: 2 weeks
- Part 1(b): Diabetic nephropathy. Approximate interval between onset and death: 3 years
- Part 1(c): Type 2 diabetes mellitus. Approximate interval between onset and death: 10 years
- Parts 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Chronic obstructive pulmonary disease, coronary artery disease. Approximate interval between onset and death: 3 years, 12 years
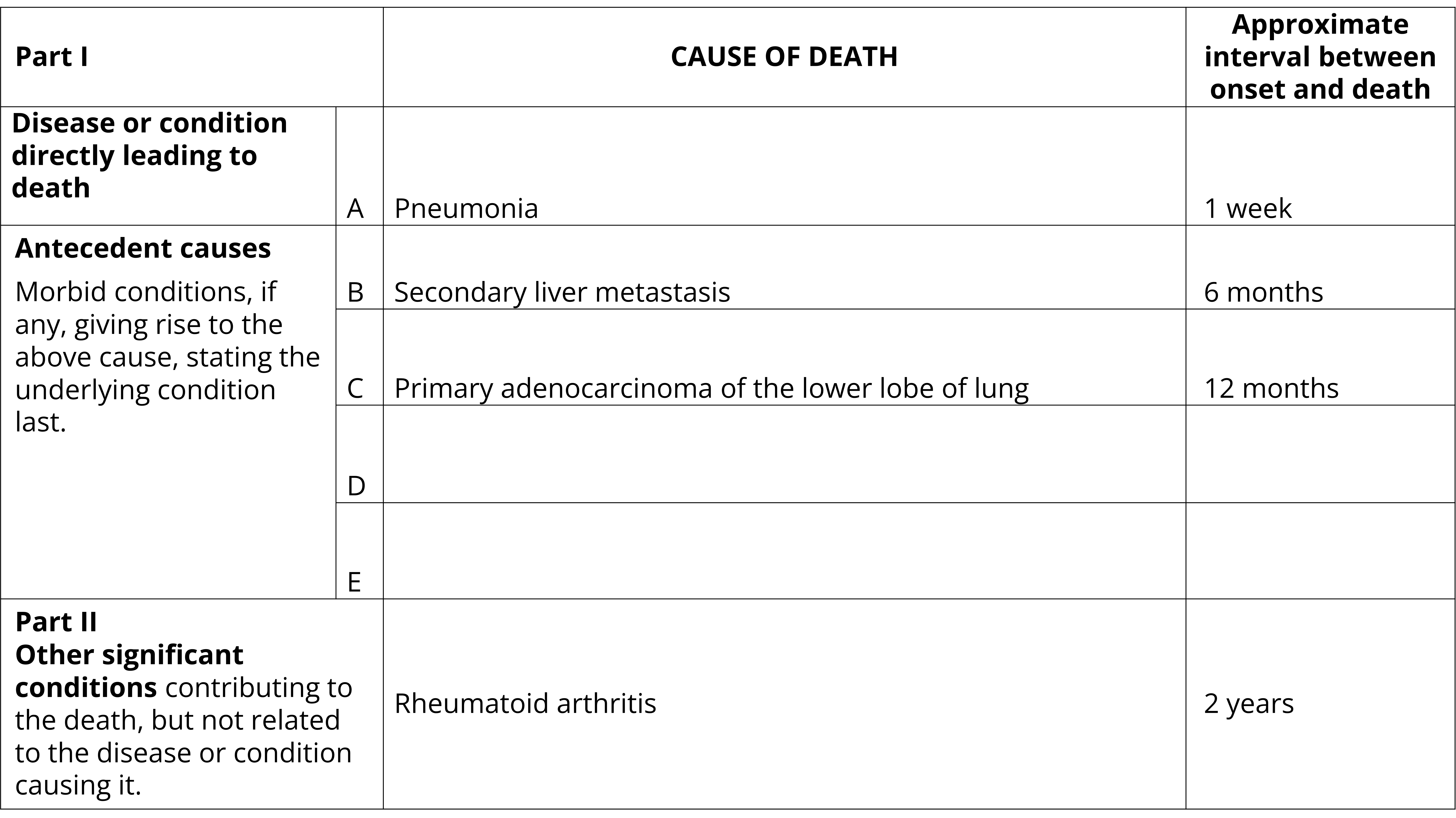
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Pneumonia. Approximate interval between onset and death: 1 week
- Part 1(b): Secondary liver metastasis. Approximate interval between onset and death: 6 months
- Part 1(c): Primary adenocarcinoma of the lower lobe of lung. Approximate interval between onset and death: 12 months
- Parts 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Rheumatoid arthritis. Approximate interval between onset and death: 2 years
Surgical and medical procedures
In most jurisdictions, deaths related to health care must be reported to the Coroner for investigation. A health care related death is one where both the health care (or failure to provide health care) caused or contributed to death and the health care was not expected to cause death. Please refer to Deaths to be reported to the coroner.
Certification principles
- When entering a post operative complication, or a complication of a medical procedure, always include the condition for which the operation was performed and when the operation was performed.
- Only include a surgery or medical procedure if there is a resultant complication. The complication should also be certified and linked to the surgical or medical procedure.
- If a surgery or medical procedure caused a complication that contributed to death, these should be certified in the cause of death of death frame of the MCCD (either Part 1 or Part 2, depending on the circumstance). These can also be entered into the surgery/procedure box on the certificate if desired. However, if the surgery, medical procedure or complication are not included in the cause of death frame it is difficult at times to understand if this has been a causal factor in the death.
The following example shows how to accurately certify a death where a procedure has led to a complication.
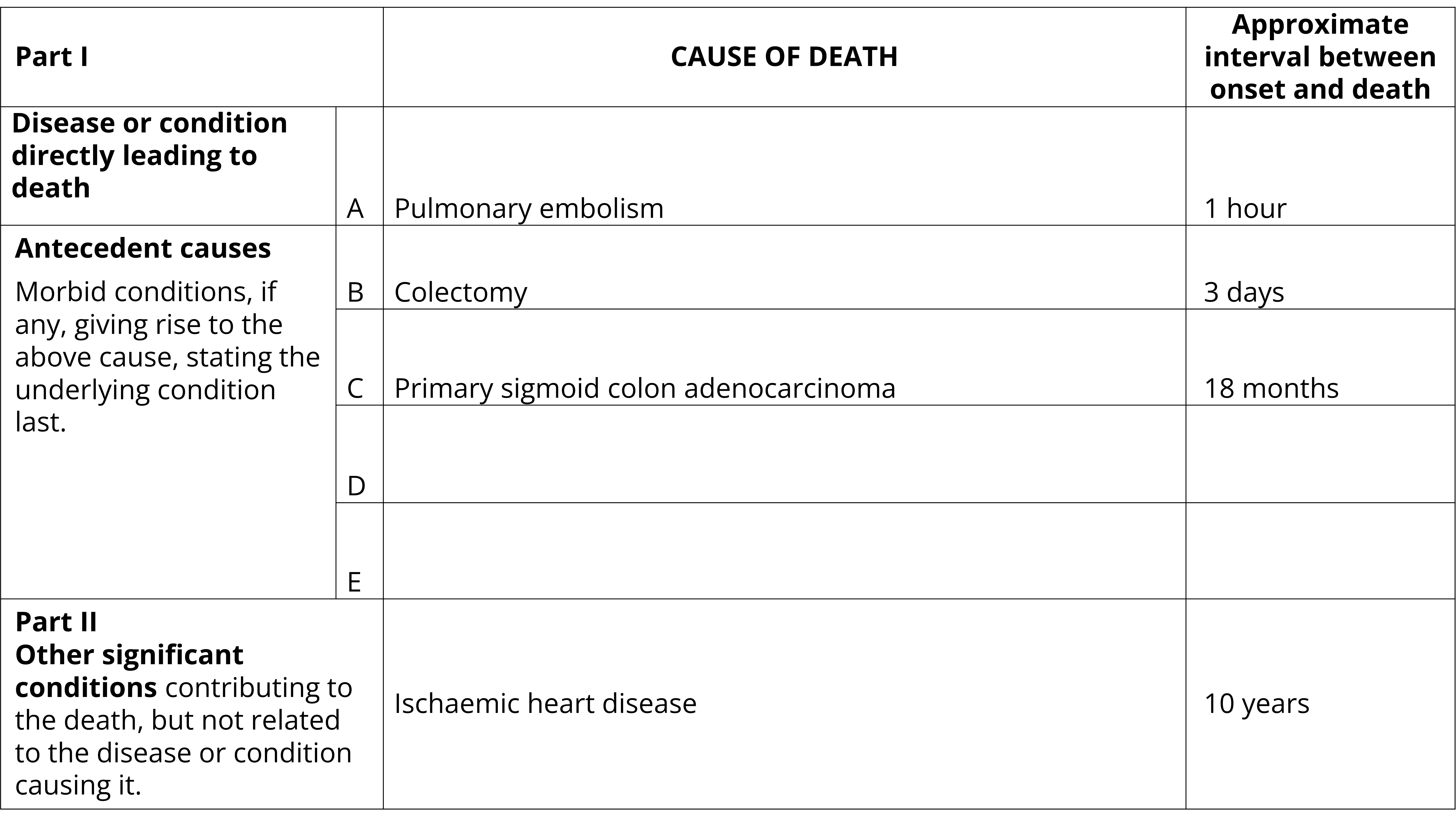
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Pulmonary embolism. Approximate interval between onset and death: 1 hour
- Part 1(b): Colectomy. Approximate interval between onset and death: 3 days
- Part 1(c): Primary sigmoid colon adenocarcinoma. Approximate interval between onset and death: 18 months
- Parts 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Ischaemic heart disease. Approximate interval between onset and death: 10 years
Prophylactic medical treatments
The same principles for certifying surgical and medical procedures apply to certifying other medical treatments including those of a prophylactic nature. In recent years the ABS has received many queries on vaccines – namely whether the vaccine should be included on the MCCD and, if so, how should it be certified. Deaths due to vaccines are rare and it is important that correct procedures are followed. The below guidance can be applied to the certification of all prophylactic medical treatments if they have caused a complication contributing to or causing death.
- Check that the death should not be referred to the coroner. In the overwhelming majority of cases, these deaths would not be expected and should be referred for a coronial investigation.
- Ensure that a complication has occurred and that this complication has caused or contributed to death.
- Enter into Part 1 or Part 2 of the MCCD. Clearly certify the complication.
- Do not record any incidental treatments or measures in either the certificate frame or the surgery/procedure box.
The following example demonstrates the above principles. Note, that a complication that has contributed to death is clearly certified.
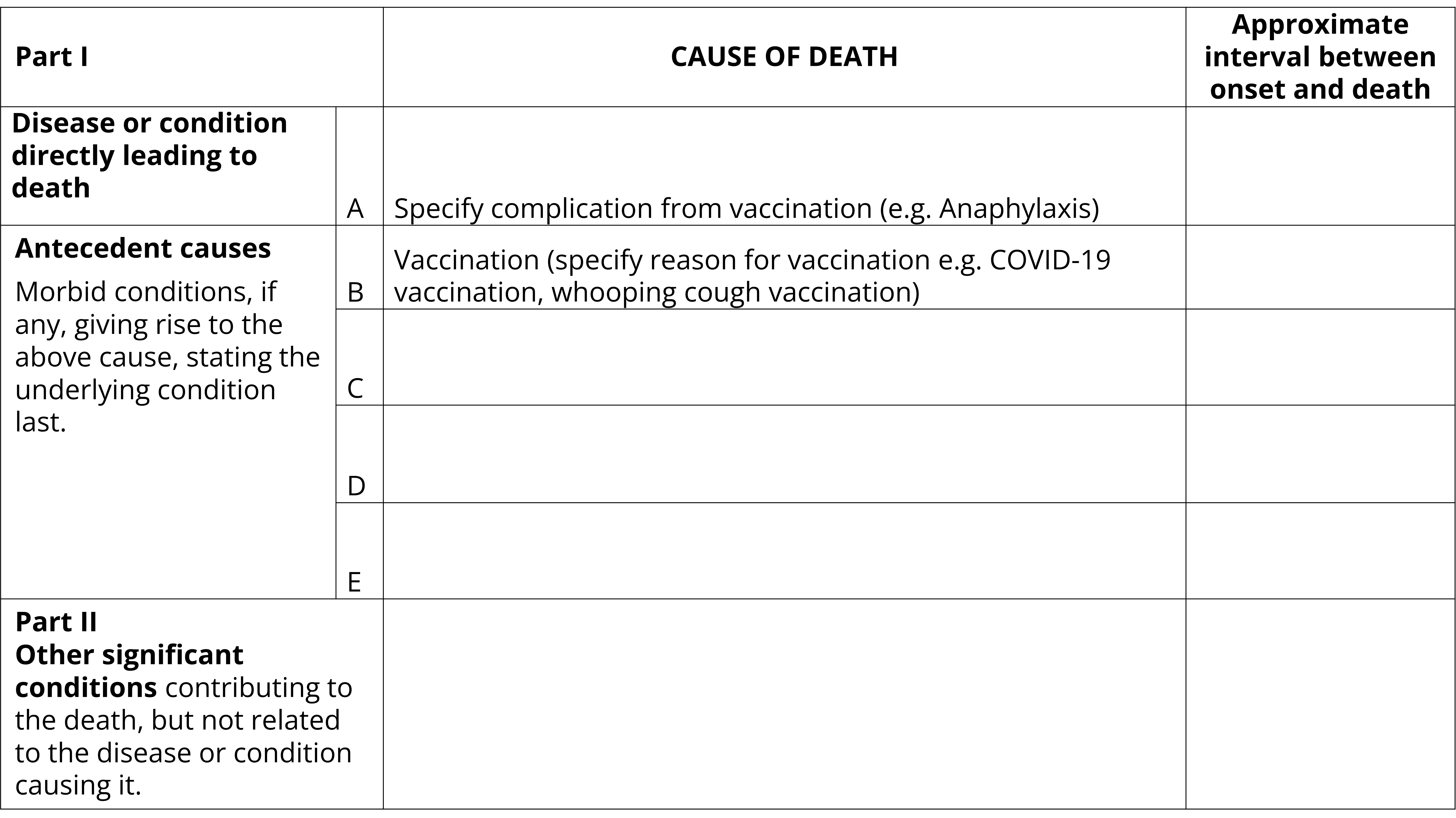
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Specify complication from vaccination (e.g. Anaphylaxis). Approximate interval between onset and death: Blank
- Part 1(b): Vaccination (specify reason for vaccination e.g. COVID-19 vaccination, whooping cough vaccination). Approximate interval between onset and death: Blank
- Part 1(c): Primary sigmoid colon carcinoma. Approximate interval between onset and death: 18 months
- Parts 1(c), 1(d), 1(e) and 2: Blank. Approximate interval between onset and death: Blank
Causes requiring further specification
Where specificity is available, the conditions listed below require at least one of the qualifying terms to provide necessary details for identification of the underlying cause of death. Certifiers should be as specific as possible when certifying all conditions, not just those listed below. The list below shows examples of the types of qualifying terms that should be used to ensure sufficient specificity for identification of the underlying cause of death.
| Condition | Qualifying terms that should be used where applicable |
|---|---|
| Dementia | Alzheimer’s disease, vascular dementia, frontotemporal dementia, Lewy body dementia, dementia due to alcohol abuse, unspecified dementia |
| Diabetes | Type 1 diabetes mellitus, type 2 diabetes mellitus, gestational diabetes |
| Stroke | Cerebral infarction, cerebral haemorrhage, subarachnoid haemorrhage, subdural haemorrhage |
| Vascular disease | Generalised arteriosclerosis, coronary artery disease, cerebrovascular disease, peripheral vascular disease, coronary atherosclerosis |
| Valve disorder | Mitral stenosis, mitral insufficiency, mitral regurgitation, aortic stenosis, aortic insufficiency, aortic regurgitation |
| Endocarditis | Infective endocarditis, non-infective endocarditis |
| Chronic respiratory conditions | Emphysema, bronchiectasis, asthma, interstitial pulmonary fibrosis, chronic bronchitis, asbestosis |
| Kidney disease | Chronic kidney disease (enter stage if known), acute kidney disease, glomerulonephritis, acute tubular necrosis, hypertensive nephropathy |
Clinical diagnosis
The conditions listed on the MCCD should be the certifier's best medical opinion as to the as to the sequence of events leading to death. There may be times where a medical diagnosis is not possible. In these instances, it is acceptable to record a clinical diagnosis where this aligns with the certifier's best medical opinion. Where a clinical diagnosis is used, the following terms are acceptable: 'clinical diagnosis of,' 'likely,' or 'probable'. For example, the following terms are acceptable terminology:
- 'Lung mass - likely primary malignancy'.
- 'Clinical diagnosis of primary lung cancer'.
- 'Probable primary site of lung carcinoma'.
The following terms should not be written on the MCCD:
- 'Querying'. When the term 'querying' appears on the MCCD it is not clear if this is a clinical diagnosis or if laboratory tests are pending.
- 'Pending tests'. When this term appears it is not clear as to whether this condition should be included as a contributory cause of death.
- The use of '?' after a term. It is not clear if this is a clinical diagnosis or if laboratory tests are pending.
Ill-defined conditions
Ill-defined or non-specific conditions should not be reported alone on a certificate without another specified condition listed on the certificate. Ill-defined conditions should not be reported as the underlying cause of death. For example, cardiac arrest is considered an ill-defined condition. Cardiac arrest must not be reported alone or as the underlying cause of death without other further specified conditions indicating the cause or train of events which resulted in the cardiac arrest.
The list below highlights some examples of ill-defined conditions that should not be reported alone or as the underlying cause of death.
- Anuria
- Ascites
- Bradycardia
- Cardiac arrest
- Collapse
- Coma
- Constipation
- Cough
- Diarrhoea
- Dysphagia
- Fever
- Frailty
- Debility
- Haemoptysis
- Haemorrhage
- Headache
- Incontinence
- Infection
- Mass (intestinal, neck, head)
- Multi-organ failure
- Natural causes
- Nausea and vomiting
- Pain
- Paralysis
- Rash
- Respiratory failure
- Senility
- Syncope
- Tachycardia
Old age
Old age should be certified as the only cause on the MCCD in rare circumstances. The age of the deceased should not be the only factor used when determining a death is due to old age. Things to consider include:
- The medical history of the deceased.
- Any known chronic conditions or injuries which have contributed to death. These must be certified on the MCCD.
- An ongoing decline in the deceased’s health due to ageing should be noted.
- Where a very elderly person dies suddenly or unexpectedly, it may be insufficient to write 'old age'. Provided a clinician feels comfortable that the death is from natural causes and not notifiable to the coroner due to concerns for a specific reason, the clinician may consider what was the most likely cause of death. Where a clinician is still unsure, advice should be sought.
Natural causes
Deaths should not be certified with ‘natural causes’ as the only condition listed on the certificate. It is important that the specific natural causes being referenced are listed on the certificate.
For some coroner referred deaths, the cause of death may still be unknown after completion of forensic pathology where there is nothing to suggest that the death is due to anything other than natural causes. If the natural causes are known these should be certified (a clinical diagnosis here is acceptable, for example, that it is likely that death was due to the effects of ischaemic heart disease). If the specific diseases are not known or there is insufficient information for certification, the cause of death should say 'unascertained natural causes'.
Conditions unlikely to cause death
Some conditions are considered unlikely to cause death. These conditions should not be certified on the MCCD alone and in most circumstances should not be reported on the lowest used line of the MCCD as the underlying cause of death. The only exceptions to this are rare circumstances where the condition has caused severe outcomes initiating a train of events leading to death or there has been an adverse outcome from a procedure/medication performed for a condition unlikely to cause death.
See Volume 2, Annex 7.4 of the ICD-10 for a list of trivial conditions unlikely to cause death that should not be used as the underlying cause.
The following example shows how a condition that may be considered unlikely to cause death may be certified.
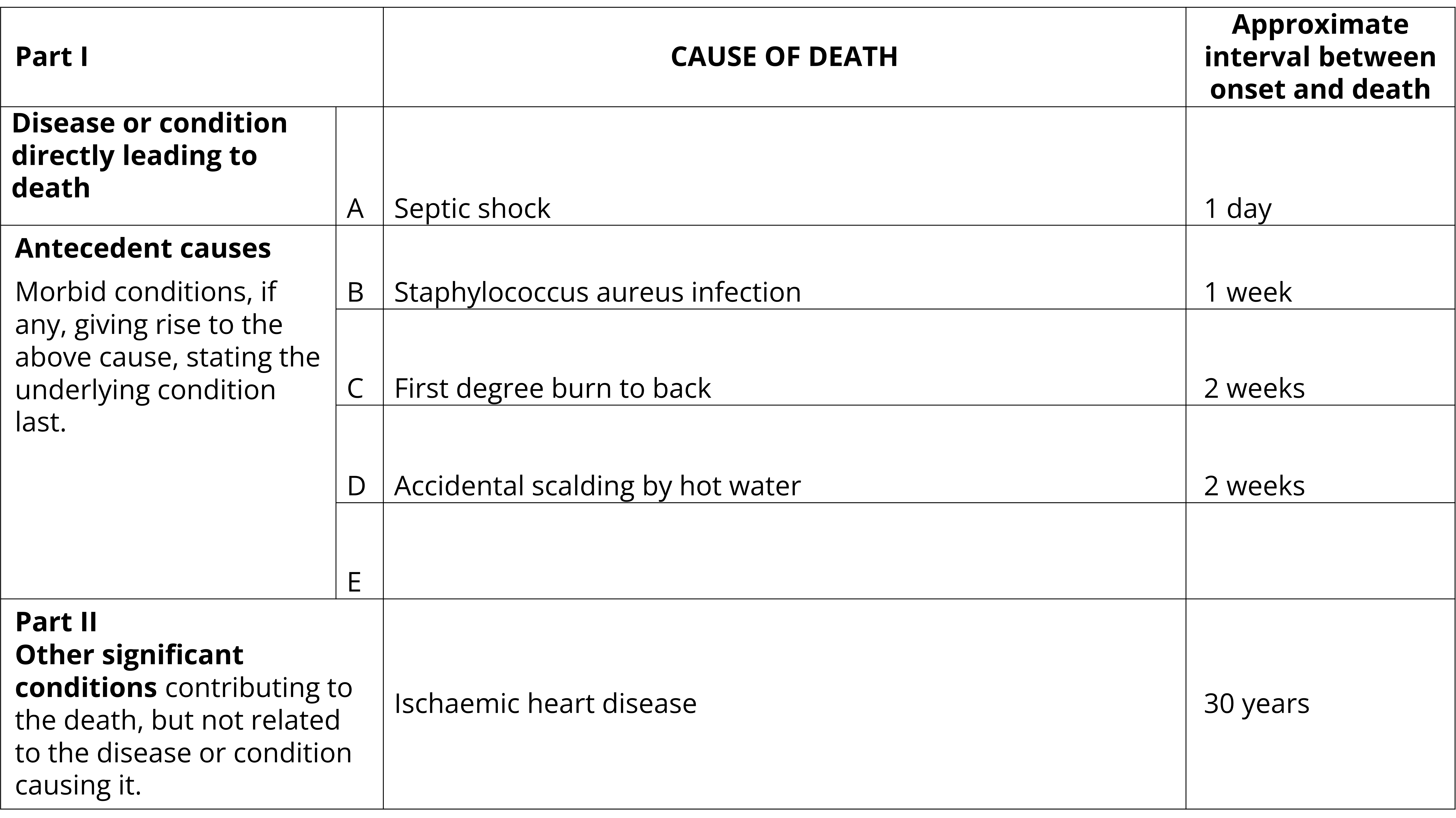
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Septic shock. Approximate interval between onset and death: 1 day
- Part 1(b): Staphylococcus aureus infection. Approximate interval between onset and death: 1 week
- Part 1(c): First degree burn to back. Approximate interval between onset and death: 2 weeks
- Part 1(d): Accidental scalding by hot water. Approximate interval between onset and death: 2 weeks
- Parts 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Ischaemic heart disease. Approximate interval between onset and death: 30 years
Common certification issues
Common certification issues
The role of the ABS is to produce statistical outputs by applying ICD-10 codes to the conditions recorded on the Medical Certificate of Cause of Death. The ABS utilises ICD-10 coding rules to assign an underlying cause of death. The following sections outline common issues with death certification which can make application of ICD-10 codes and coding rules difficult including:
- Cancer and neoplasms
- Dementia
- Infectious diseases
- Acute respiratory infections including COVID-19, Influenza and Respiratory Syncytial virus
- External causes
- Fractures
- Skin conditions
- Rare conditions
- Pulmonary embolism
- Renal failure
Cancer and neoplasms
Certification of cancer and neoplasms
Neoplasms are classified by site, behaviour and morphology. This information is used to assign the appropriate ICD code to the neoplasm. Insufficient information can lead to the incorrect assignment of a term. For example, terms such as 'neoplasm', 'mass,' 'growth' and 'tumour' should not be used without qualification as to whether malignant or benign.
Common issues with certification of neoplasms include:
- Not stating the site of the neoplasm.
- Not stating the behaviour of the neoplasm. For example, sometimes a term such as 'brain tumour' is used interchangeably with 'brain cancer'. If a brain cancer such as a frontoparietal glioblastoma is described as a 'brain tumour' it will be assigned as a benign tumour rather than a malignancy.
- Lack of clarity of whether the cancer is primary or secondary. The term 'metastatic lung cancer' may mean that the cancer has metastasised from the lung or it may mean that it has metastasised to the lung. It is important to clarify if a cancer is primary or secondary.
- The use of broad terms to describe multiple sites resulting in poor specificity such as 'bowel cancer', 'head and neck cancer', or 'oral cancer'. Further specificity is required to identify the exact site.
The following guidelines should be followed:
| Term | Specificity required |
|---|---|
| Behaviour | Malignant, benign, in situ, unknown behaviour. If malignant: clearly define if cancer is primary or secondary. |
| Site | Always state the exact site if known (do not use broad terms to encompass a site). |
| Morphology | If known, specify histological classification of the tissue. |
The following terms should not be used:
| Do not use terms in this column | Use instead |
|---|---|
| Head and neck cancer | Specify precisely if skin surface or other site e.g. skin of lip, skin of eyelid, skin of ear, skin of scalp, skin of neck, inner cheek, base of tongue, dorsal surface of tongue, gum, salivary gland, nasopharynx, hypopharynx, pyriform sinus, etc. |
| Bowel cancer | Specify exact site e.g. colon cancer, sigmoid colon cancer, cancer of rectosigmoid junction, etc. |
| Abdominal cancer | Specify exact site e.g. body of stomach, gastro-oesophageal junction, pylorus, etc. |
| Squamous cell carcinoma | Specify precisely if skin surface or other site e.g. squamous cell carcinoma of lung, squamous cell carcinoma of skin of face, squamous cell carcinoma skin of lip, etc. |
| Neuroendocrine cancer | Specify site e.g. neuroendocrine carcinoma of lung, etc. |
| Melanoma | Specify site e.g melanoma of eye (orbit, ocular, etc), vulvar melanoma, scrotal melanoma, etc. |
| Transitional cell carcinoma | Specify site e.g. transitional cell carcinoma of kidney, transitional cell carcinoma of bladder, transitional cell carcinoma of ureter, etc. |
Certifying primary cancers
- The primary site should always be indicated, even though the primary growth may have been removed long before death. If a secondary growth is included in the sequence of events leading to death, record the site of the secondary growth due to the site of the primary growth.
- If the primary site is unknown, this must be stated on the certificate.
- Avoid using broad terms set out in the table above.
- Add as much specification as possible to the site as set out in the table below.
- Clearly differentiate between primary and secondary cancers on the certificate.
- If there are multiple primary sites, certify all sites individually. Do not use 'multiple primaries'.
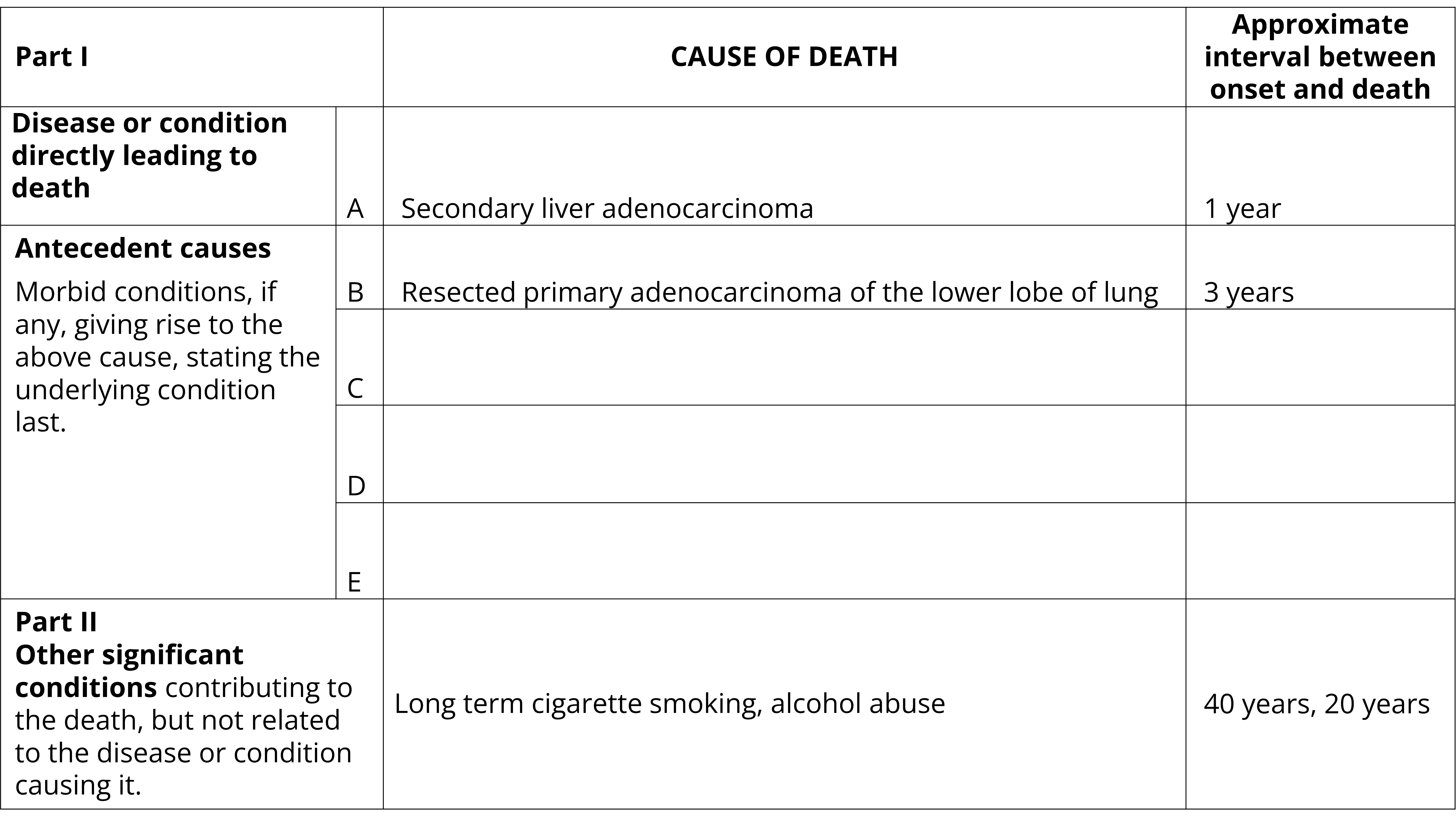
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Secondary liver adenocarcinoma. Approximate interval between onset and death: 1 year
- Part 1(b): Resected primary adenocarcinoma of the lower lobe of lung. Approximate interval between onset and death: 3 years
- Parts 1(c), 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Long term cigarette smoking, alcohol abuse. Approximate interval between onset and death: 40 years, 20 years
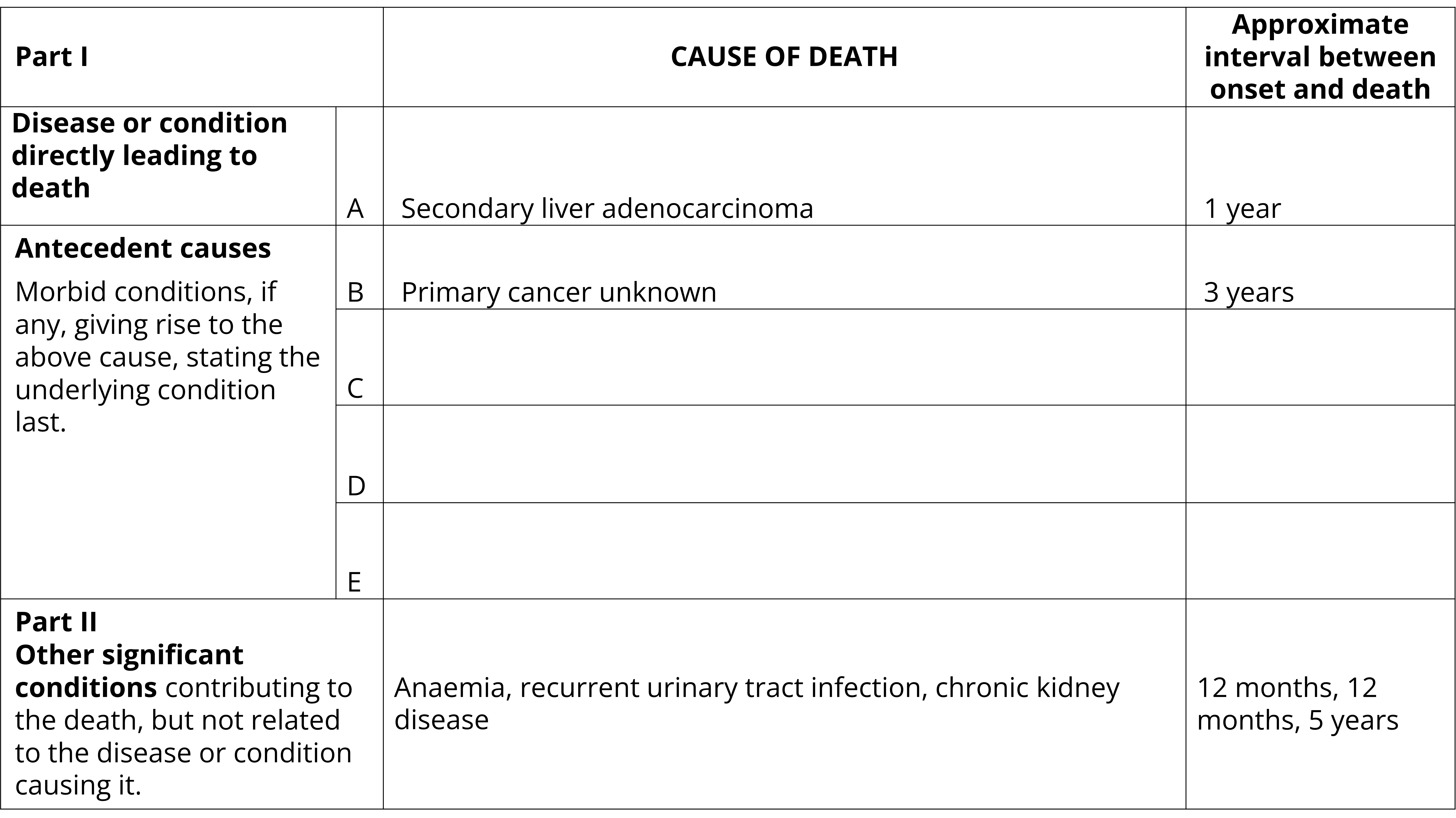
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Secondary liver adenocarcinoma. Approximate interval between onset and death: 1 year
- Part 1(b): Primary cancer unknown. Approximate interval between onset and death: 3 years
- Parts 1(c), 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Anaemia, recurrent urinary tract infection, chronic kidney disease. Approximate interval between onset and death: 12 months, 12 months, 5 years
Specificity of neoplasm sites
To provide the details for identification of the underlying cause of death, the primary neoplasm sites listed in the table below require at least one of the qualifying terms (where specificity is available). Certifiers should be as specific as possible when certifying the site of any neoplasm, not just those sites listed below.
The four examples after the table show how deaths due to cancer may be certified. In the examples, the site of the cancer is clearly specified as well as whether the cancer is primary or secondary.
| Site | Subsite to be specified where applicable | Examples of subtype or other qualifying terms to be used where applicable |
|---|---|---|
| Lip | Lower, upper, commissure, skin of lip, overlapping | Squamous cell carcinoma |
| Mouth | Cheek (mucosa), vestibule, retro molar, overlapping | Squamous cell carcinoma |
| Pharynx | Nasopharynx, hypopharynx, oropharynx, tonsil, pyriform sinus, overlapping | Squamous cell carcinoma |
| Oral | Tongue, salivary gland, palate, gum, overlapping | Squamous cell carcinoma |
| Skin | Vulva, vagina, penis, scrotum, other specified site | Melanoma (by site), basal cell carcinoma (by site), squamous cell carcinoma (by site) |
| Liver | Hepatocellular, intrahepatic duct | Sarcoma, angiosarcoma, hepatoblastoma |
| Bowel | Large (colon), small, colon with rectum, sigmoid colon | |
| Uterus | Cervix uteri, corpus uteri, ligament, overlapping | |
| Endocrine gland | Parathyroid, pituitary, craniopharyngeal, pineal, aortic body, pluriglandular | |
| Adrenal gland | Medulla, cortex | |
| Respiratory | Nasal cavity, middle ear, accessory sinus, mediastinum, trachea, thymus, bronchus, larynx, overlapping | |
| Lung | Upper lobe, lower lobe, middle lobe, main bronchus, overlapping | Primary, secondary |
| Breast | Upper inner quadrant, lower inner quadrant, upper outer quadrant, axillary tail, central portion, nipple and areola, overlapping | |
| Urinary organs | Kidney, ureter, bladder, urethra, paraurethral gland, overlapping | |
| Central nervous system | Meninges, brain, 'specific' ventricle, brain stem, cranial nerve, spinal cord, cauda equina, overlapping, | Primary, secondary |
| Gastrointestinal system | Cervical part of oesophagus, thoracic part of oesophagus, abdominal part of oesophagus, gastro-oesophageal junction, fundus of stomach, body of stomach, pyloric antrum, pylorus, duodenum, jejunum, ileum, Meckel diverticulum, caecum, appendix, ascending colon, hepatic flexure, transverse colon, splenic flexure, descending colon, sigmoid colon, anal canal |
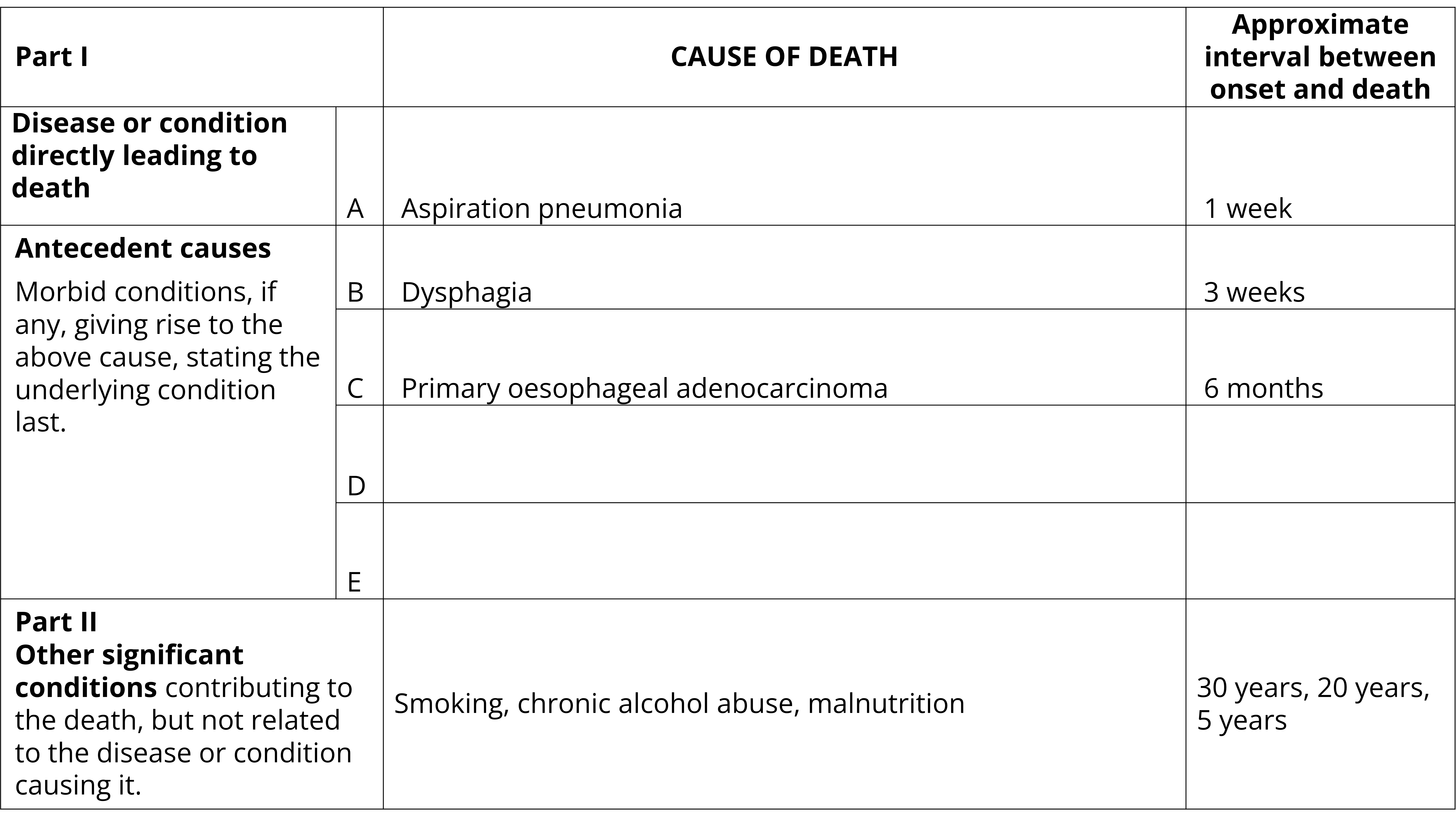
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Example of a completed Medical Certificate of Cause of Death. The certificate is filled out as follows:
- Part 1(a): Aspiration pneumonia. Approximate interval between onset and death: 1 week
- Part 1(b): Dysphagia. Approximate interval between onset and death: 3 weeks
- Part 1(c): Primary oesophageal carcinoma. Approximate interval between onset and death: 6 months
- Parts 1(d) and 1(e) Blank. Approximate interval between onset and death: Blank
- Part 2: Smoking, chronic alcohol abuse, malnutrition. Approximate interval between onset and death: 30 years, 20 years, 5 years
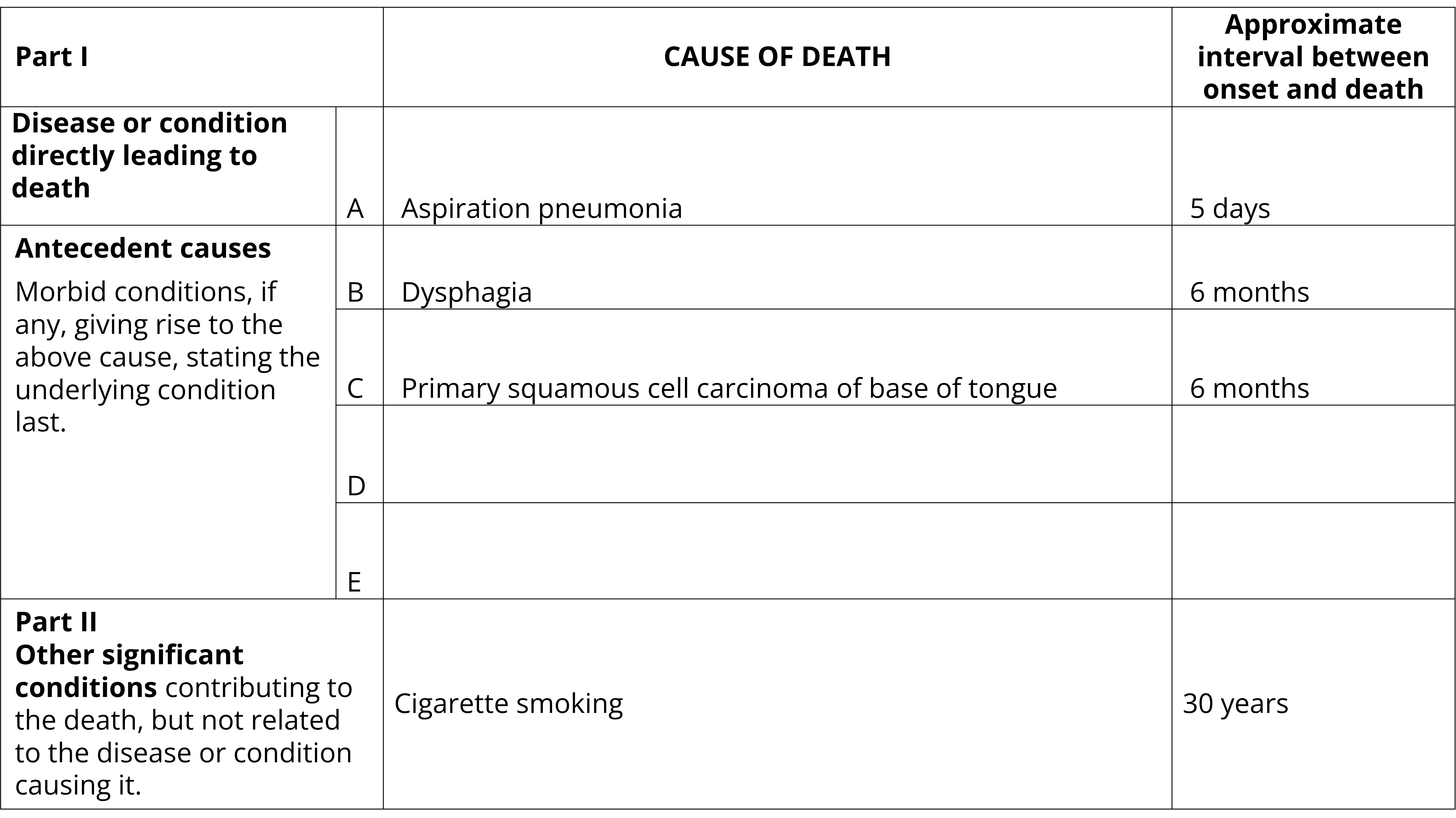
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Aspiration pneumonia. Approximate interval between onset and death: 5 days
- Part 1(b): Dysphagia. Approximate interval between onset and death: 6 months
- Part 1(c): Primary squamous cell carcinoma of base of tongue. Approximate interval between onset and death: 6 months
- Parts 1(d) and 1(e) Blank. Approximate interval between onset and death: Blank
- Part 2: Cigarette smoking. Approximate interval between onset and death: 30 years
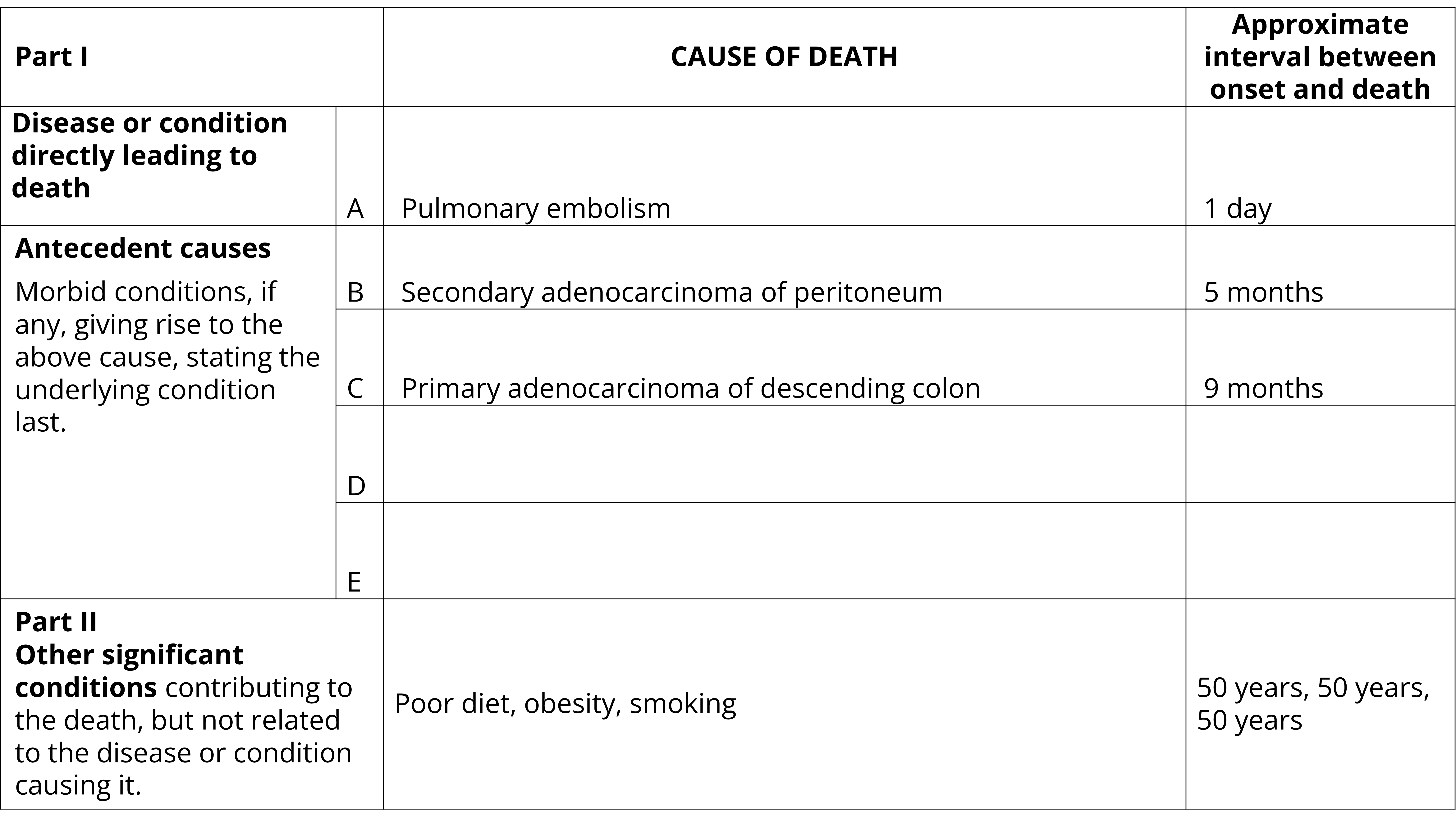
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Pulmonary embolism. Approximate interval between onset and death: 1 day
- Part 1(b): Secondary adenocarcinoma of peritoneum. Approximate interval between onset and death: 5 months
- Part 1(c): Primary adenocarcinoma of descending colon. Approximate interval between onset and death: 9 months
- Parts 1(d) and 1(e) Blank. Approximate interval between onset and death: Blank
- Part 2: Poor diet, obesity, smoking. Approximate interval between onset and death: 50 years, 50 years, 50 years
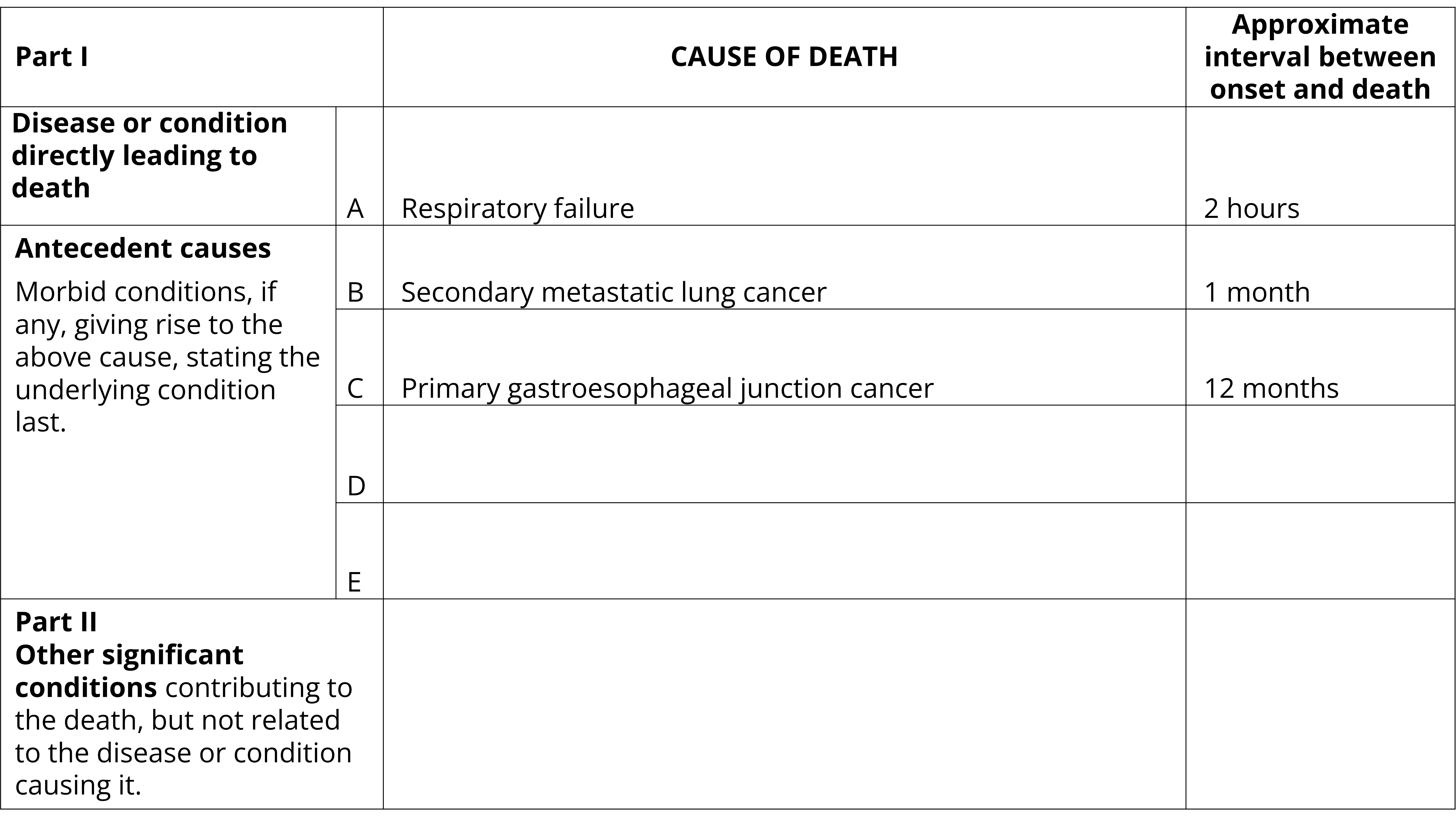
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Respiratory failure. Approximate interval between onset and death: 2 hours
- Part 1(b): Secondary metastatic lung cancer. Approximate interval between onset and death: 1 month
- Part 1(c): Primary gastroesophageal junction cancer. Approximate interval between onset and death: 12 months
- Parts 1(d), 1(e) and Part 2: Blank. Approximate interval between onset and death: Blank
Dementia
Certification of dementia
When certifying deaths due to dementia:
- If the type or cause of dementia is known this must be specified on the death certificate e.g. Alzheimer’s disease, vascular dementia, frontotemporal dementia, Lewy body dementia, dementia due to alcohol abuse.
- If the type or cause of dementia is unknown document this as 'unspecified dementia'.
Mixed dementia
If two or more types of dementia have contributed to the death, ensure both are specified on the death certificate. The following two examples show how mixed dementia may be certified.
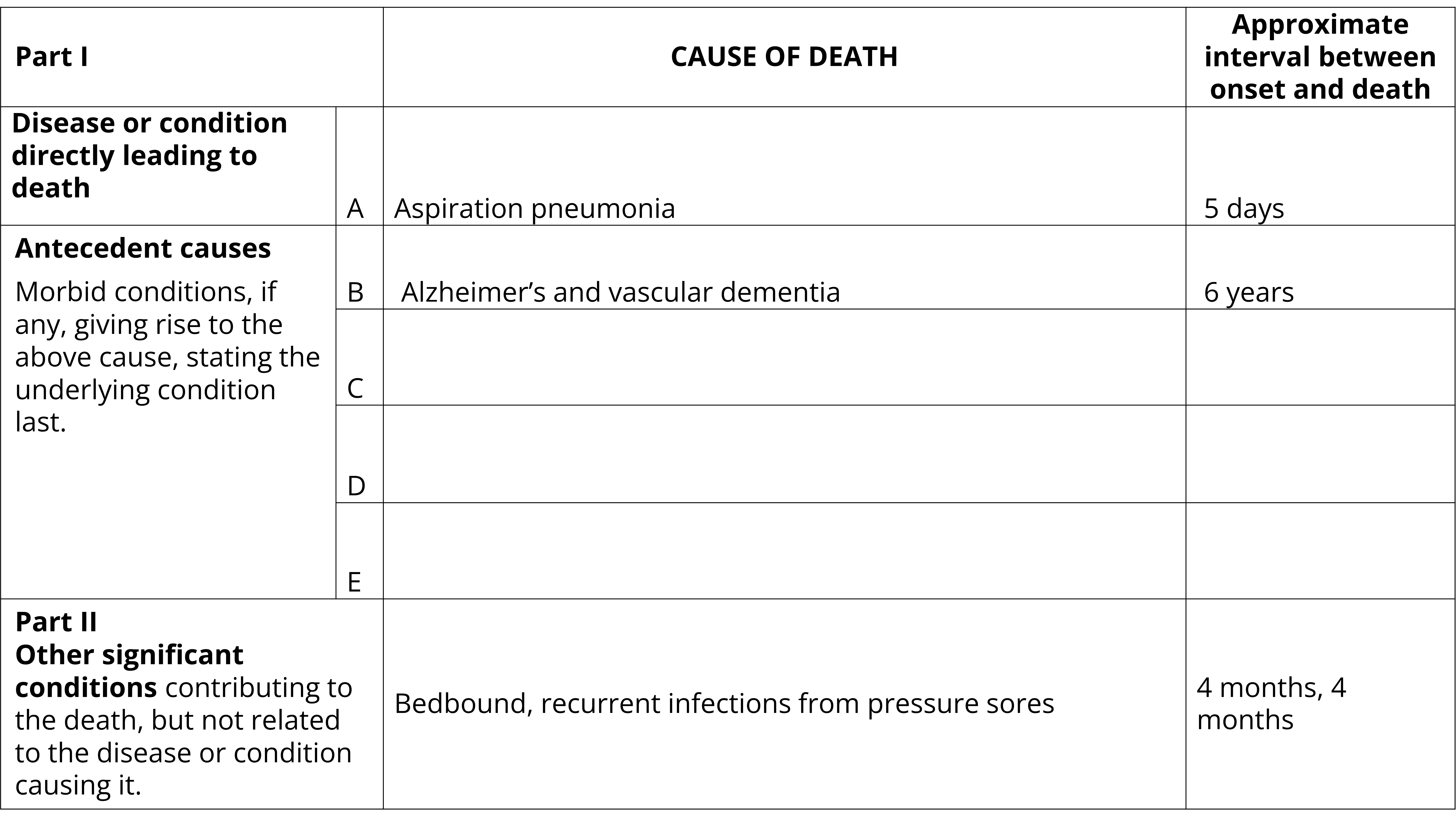
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Aspiration pneumonia. Approximate interval between onset and death: 5 days
- Part 1(b): Alzheimer’s and vascular dementia. Approximate interval between onset and death: 6 years
- Parts 1(c), 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Bedbound, recurrent infections from pressure sores. Approximate interval between onset and death: 4 months, 4 months
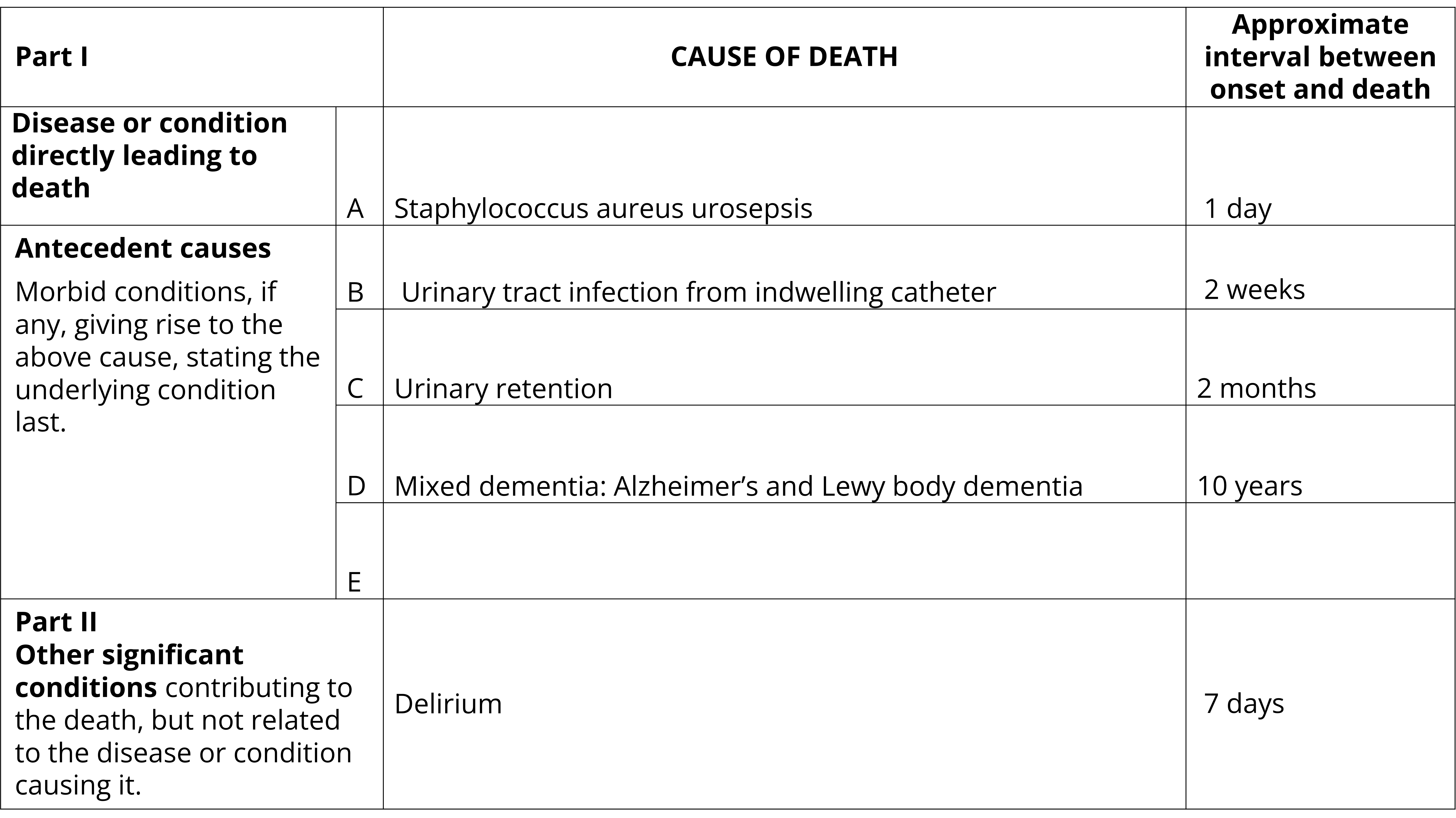
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Staphylococcus aureus urosepsis. Approximate interval between onset and death: 1 day
- Part 1(b): Urinary tract infection from indwelling catheter. Approximate interval between onset and death: 2 weeks
- Part 1(b): Urinary retention. Approximate interval between onset and death: 2 months
- Part 1(d): Mixed dementia: Alzheimer’s and Lewy body dementia. Approximate interval between onset and death: 10 years
- Part 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Delirium. Approximate interval between onset and death: 7 days
Infectious diseases
Certification of infectious or parasitic diseases
When certifying deaths due to infectious or parasitic diseases:
- Identify whether a primary infection was bacterial, viral or fungal.
- State the name of the causative agent, if the disease name does not imply this.
- Provide the site of the infection (e.g. urinary tract, respiratory tract).
- Specify the organism on the MCCD if it is known.
Sepsis and septicaemia
Where sepsis and septicaemia is the direct cause of death, certifiers should document:
- The site of the original infection.
- The causative organism.
The following example shows how more specificity can be applied to sepsis. These principles can be applied to other infections.
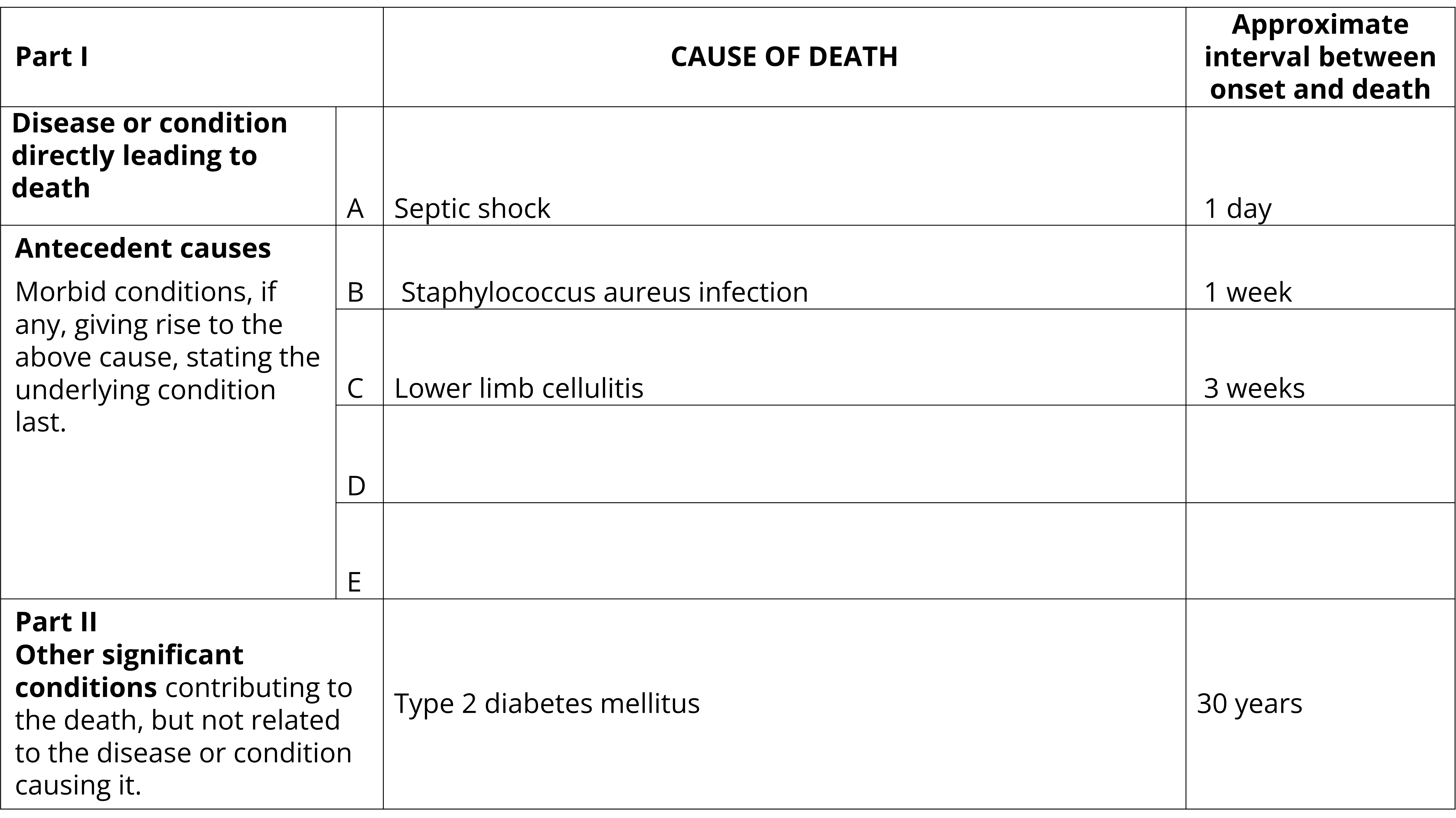
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Septic shock. Approximate interval between onset and death: 1 day
- Part 1(b): Staphylococcus aureus infection. Approximate interval between onset and death: 1 week
- Part 1(c): Lower limb cellulitis. Approximate interval between onset and death: 3 weeks
- Parts 1(d) and 1(e) Blank. Approximate interval between onset and death: Blank
- Part 2: Type 2 diabetes mellitus. Approximate interval between onset and death: 30 years
Pneumonia and bronchopneumonia
For deaths due to pneumonia or bronchopneumonia, identify:
- If the condition is viral, bacterial, fungal, primary hypostatic or due to aspiration.
- The causative organism where it is known.
- Any underlying condition that may have led to the pneumonia.
- Any condition leading to inactivity or debility, if this was the cause of the pneumonia.
The following example shows how more specifity can be added to pneumonia on the MCCD.
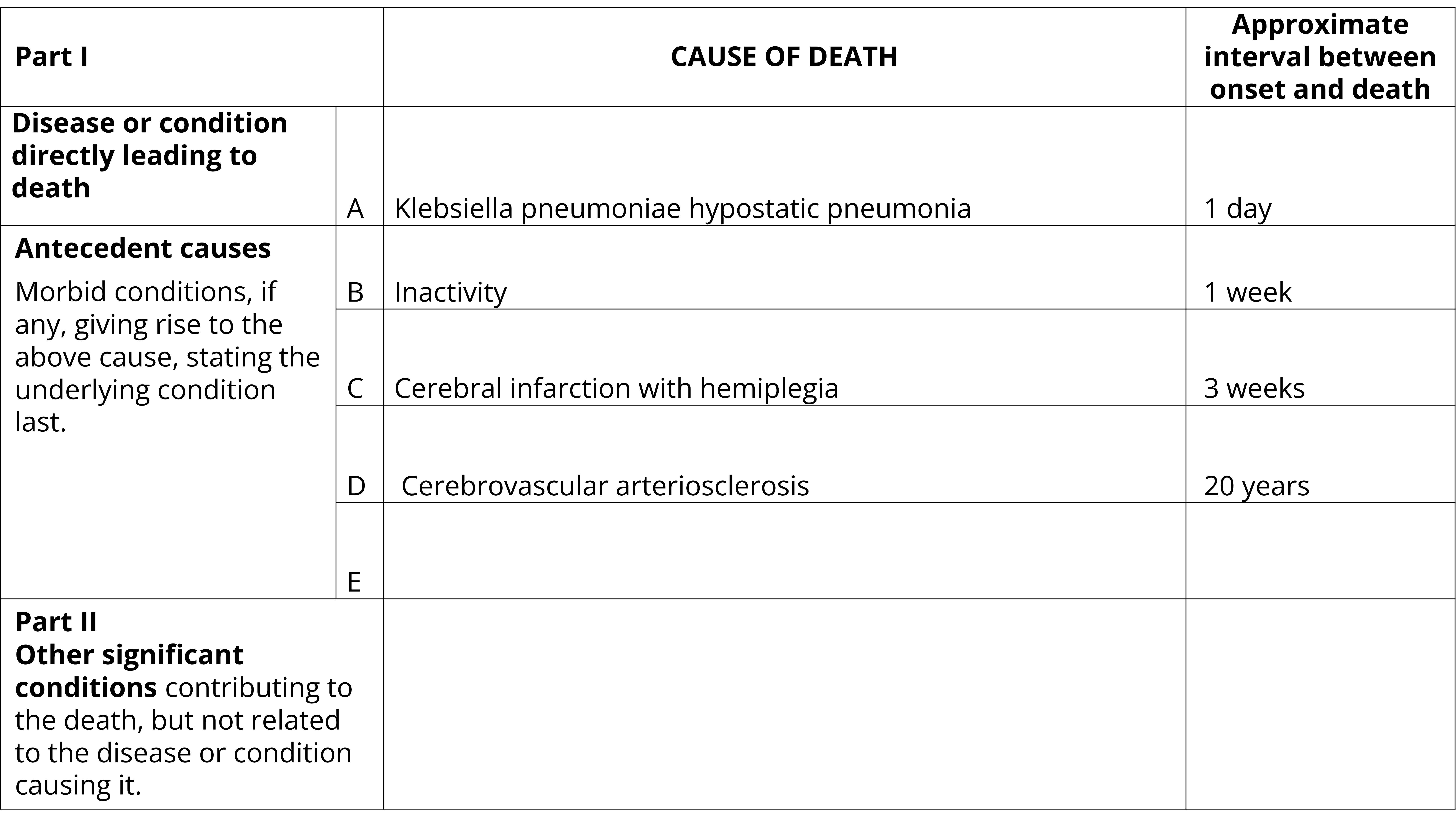
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Klebsiella pneumoniae hypostatic pneumonia. Approximate interval between onset and death: 1 day
- Part 1(b): Inactivity. Approximate interval between onset and death: 1 week
- Part 1(c): Cerebral infarction with hemiplegia. Approximate interval between onset and death: 3 weeks
- Part 1(d): Cerebrovascular arteriosclerosis. Approximate interval between onset and death: 20 years
- Parts 1(e) and Part 2: Blank. Approximate interval between onset and death: Blank
Acute respiratory infections including COVID-19, Influenza and Respiratory Syncytial virus
Terminology
Viral illnesses should be recorded on the Medical Certificate of Cause of Death (MCCD) where the disease caused, or is clinically diagnosed as having caused, or contributed to death. Viral illnesses should be recorded in Part 1 where it was a part of the chain of events leading to death. Viral illnesses should be recorded in Part 2 where they are thought to have contributed to the death but was not part of the direct chain of events leading to death.
COVID-19:
- Do not use the term coronavirus. Instead state that is was COVID-19, SARS-CoV-2, etc.
- Specify whether the infection is current or a sequelae complication (e.g. long COVID-19).
Influenza:
- State the strain if known (e.g. Influenza A, B or H1N1).
The following example demonstrates how a death due to a viral illness may be certified. The strain is clearly specified, as are complications of the virus.
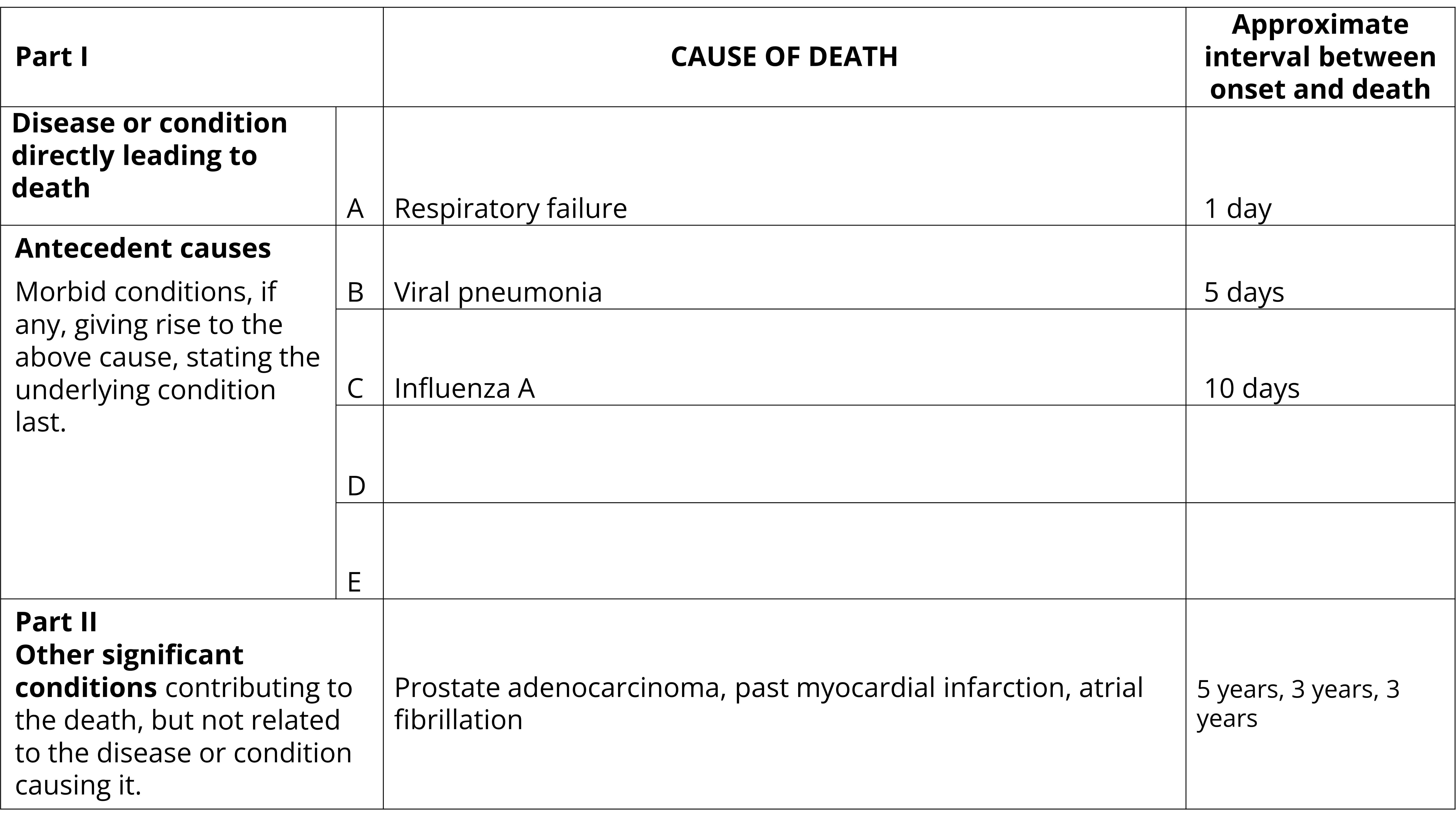
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Respiratory failure. Approximate interval between onset and death: 1 day
- Part 1(b): Viral pneumonia. Approximate interval between onset and death: 5 days
- Part 1(c): Influenza A. Approximate interval between onset and death: 10 days
- Parts 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Prostate adenocarcinoma, past myocardial infarction, atrial fibrillation. Approximate interval between onset and death: 5 years, 3 years, 3 years
Complications of viral illnesses leading to death
Specification of the causal pathway leading to death in Part 1 of the certificate is important and all conditions and symptoms should be included. For example, in cases where COVID-19 causes pneumonia and fatal respiratory distress, both pneumonia and respiratory distress should be included along with COVID-19 in Part 1. The duration of each disease and symptom should also be included. Certifiers should include as much detail as possible based on their knowledge of the case, medical records, laboratory testing, etc.
The following two examples show how complications of a viral illness can be certified.
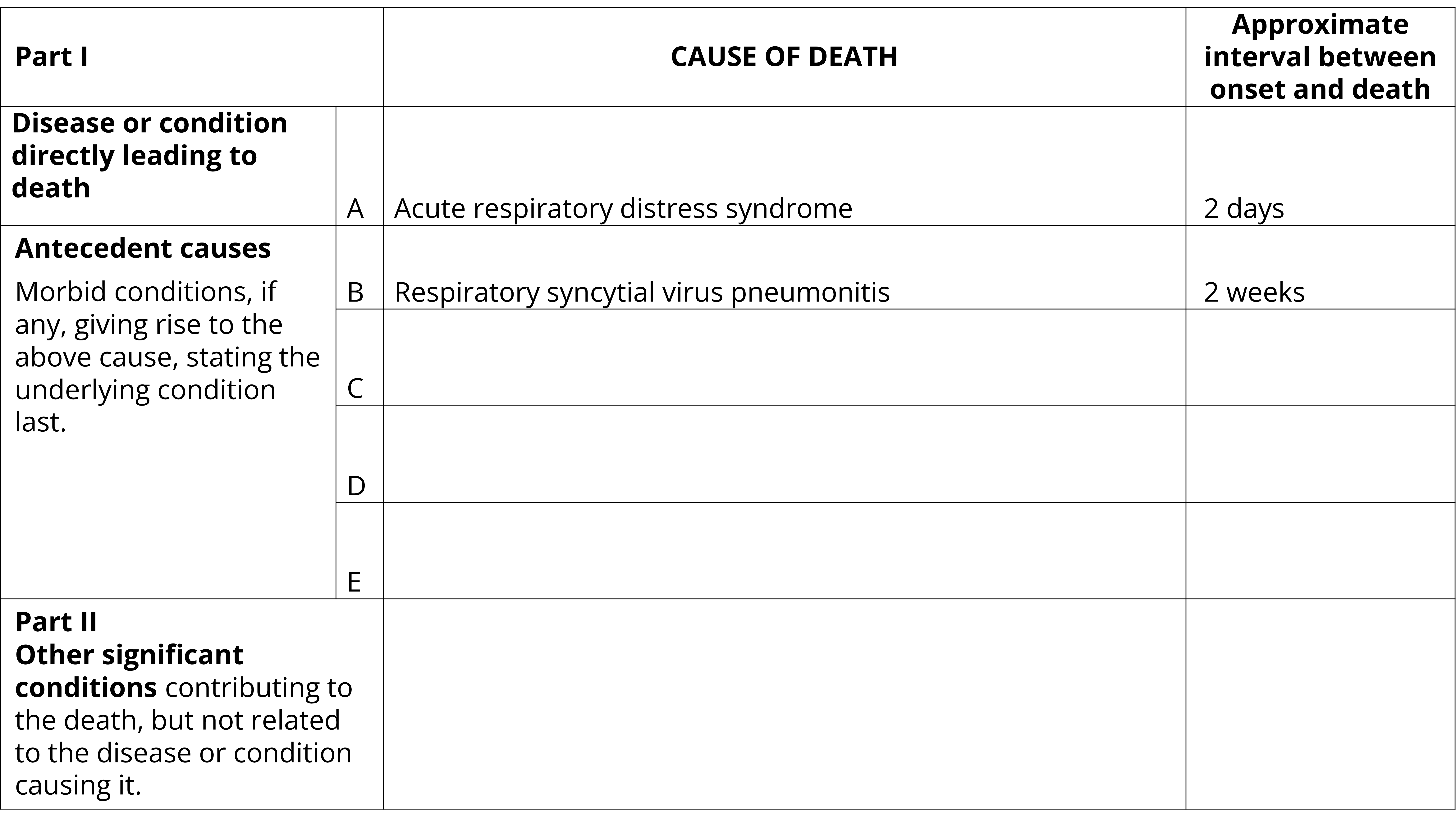
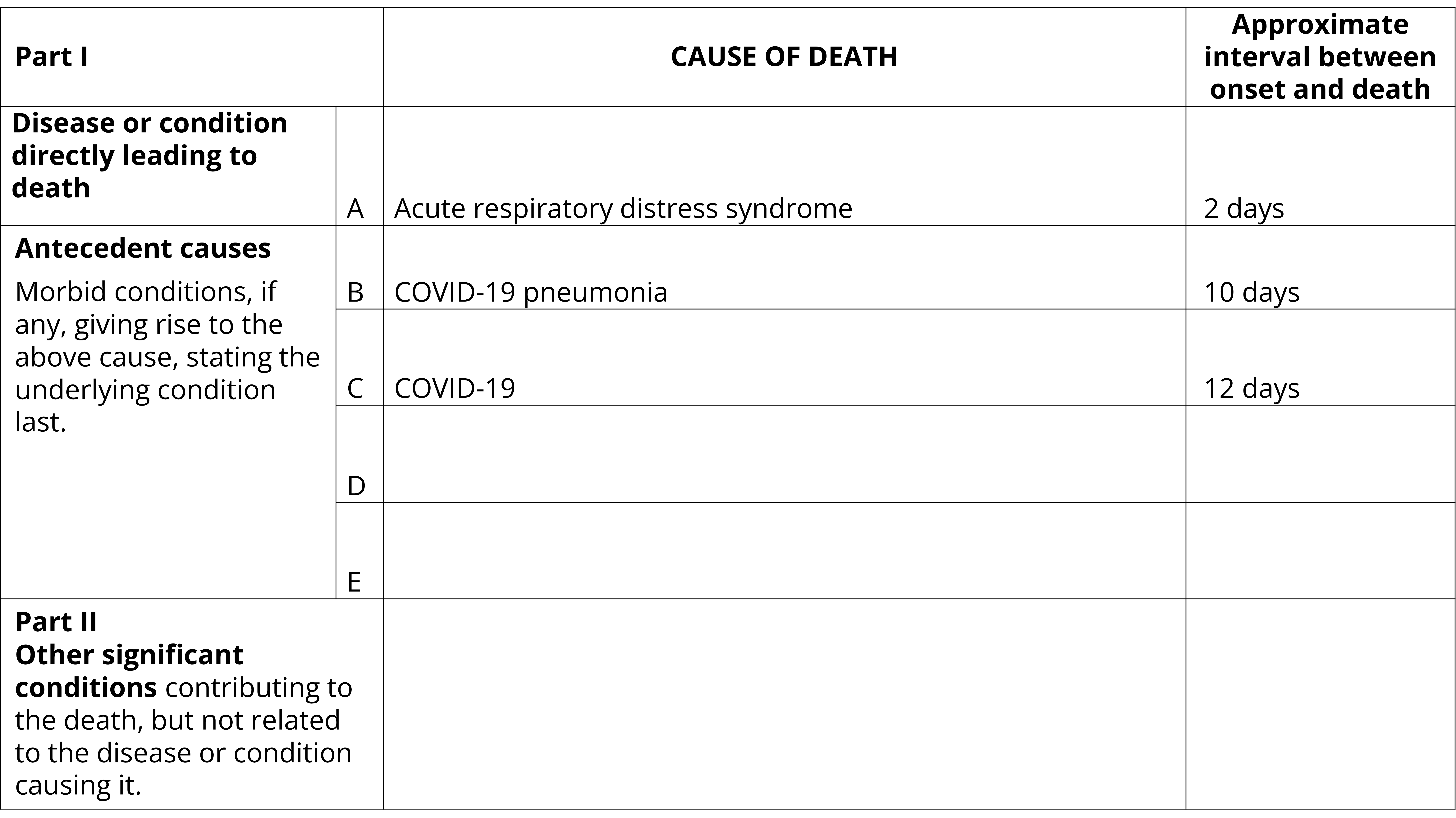
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Acute respiratory distress syndrome. Approximate interval between onset and death: 2 days
- Part 1(b): Respiratory syncytial virus pneumonitis . Approximate interval between onset and death: 2 weeks
- Parts 1(c) 1(d), 1(e) and Part 2: Blank. Approximate interval between onset and death: Blank
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Acute respiratory distress syndrome. Approximate interval between onset and death: 2 days
- Part 1(b): COVID-19 pneumonia. Approximate interval between onset and death: 10 days
- Part 1(c): COVID-19. Approximate interval between onset and death: 12 days
- Parts 1(d), 1(e) and Part 2: Blank. Approximate interval between onset and death: Blank
Viral illnesses with co-morbidities
Existing conditions, especially those which are chronic in nature, may have also contributed to death and should be certified in Part 2 of the MCCD. Chronic conditions may include but are not limited to coronary artery disease, chronic obstructive pulmonary disease, diabetes, cancer or disabilities.
The following three examples show how comorbidities may be certified on the MCCD for deaths due to acute respiratory illnesses.
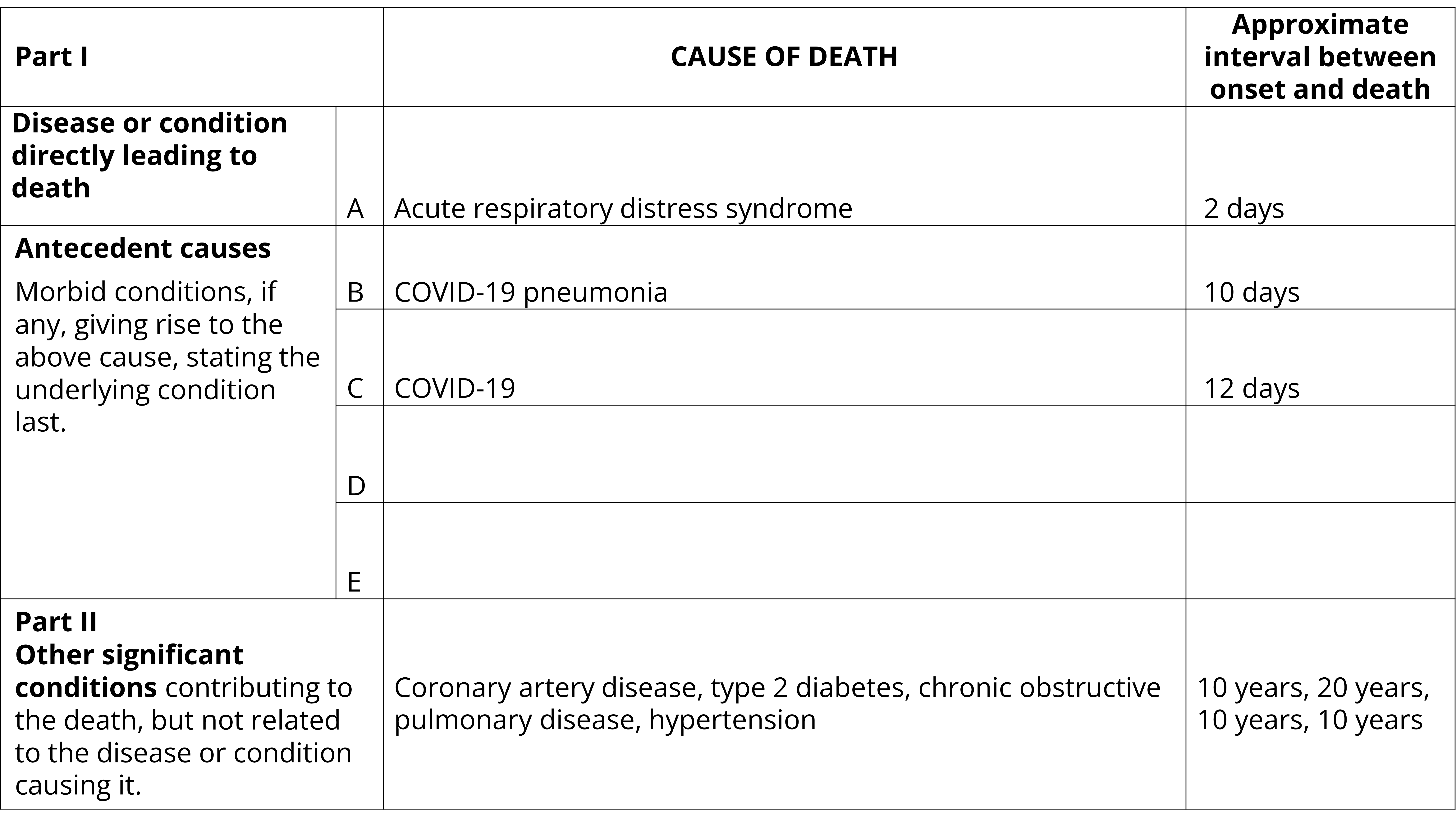
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Acute respiratory distress syndrome. Approximate interval between onset and death: 2 days
- Part 1(b): COVID-19 pneumonia. Approximate interval between onset and death: 10 days
- Part 1(c): COVID-19. Approximate interval between onset and death: 12 days
- Parts 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Coronary artery disease, type 2 diabetes, chronic obstructive pulmonary disease, hypertension. Approximate interval between onset and death: 10 years, 20 years, 10 years, 10 years
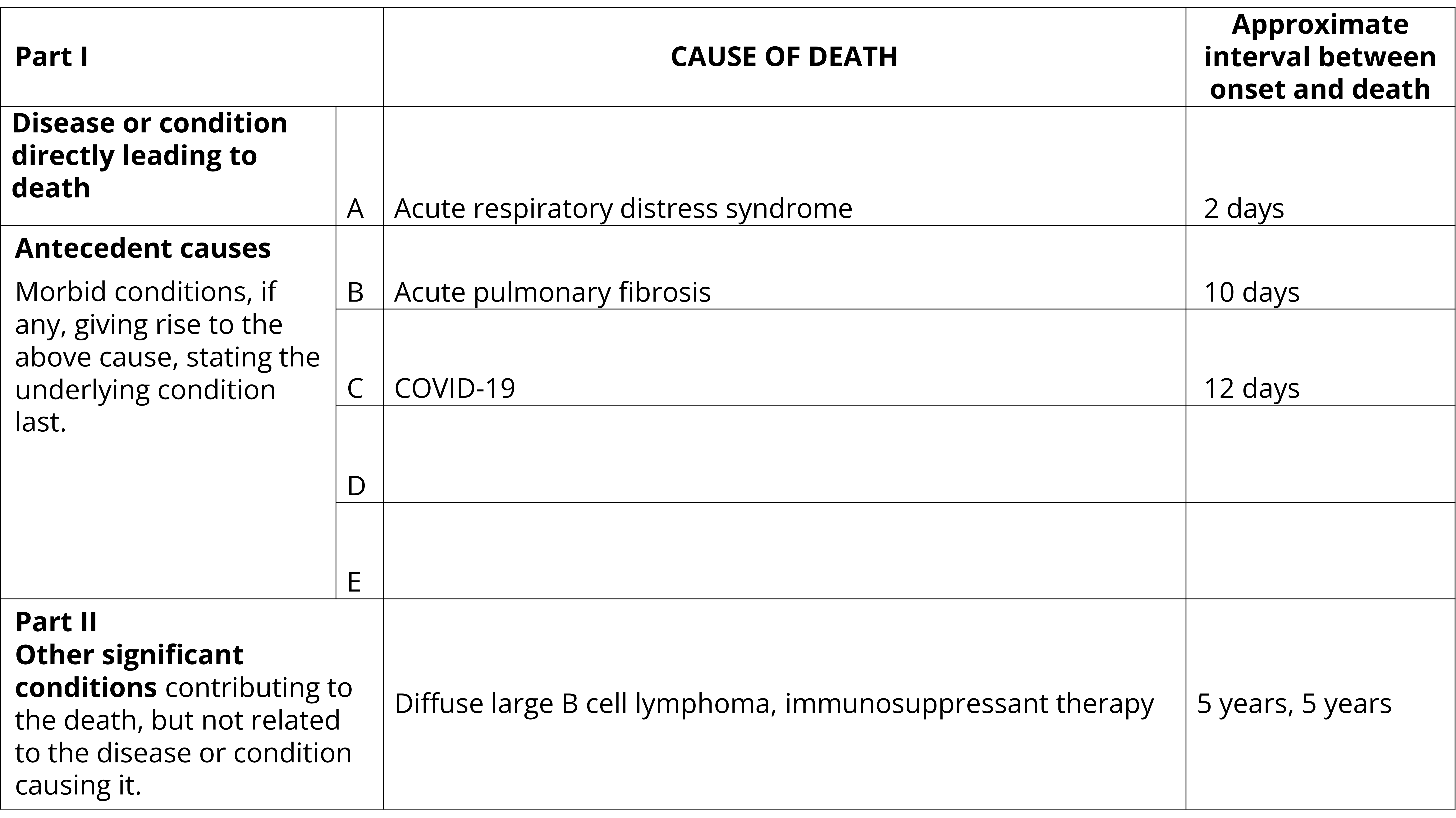
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Acute respiratory distress syndrome. Approximate interval between onset and death: 2 days
- Part 1(b): Acute pulmonary fibrosis. Approximate interval between onset and death: 10 days
- Part 1(c): COVID-19. Approximate interval between onset and death: 12 days
- Parts 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Diffuse large B cell lymphoma, immunosuppressant therapy. Approximate interval between onset and death: 5 years, 5 years
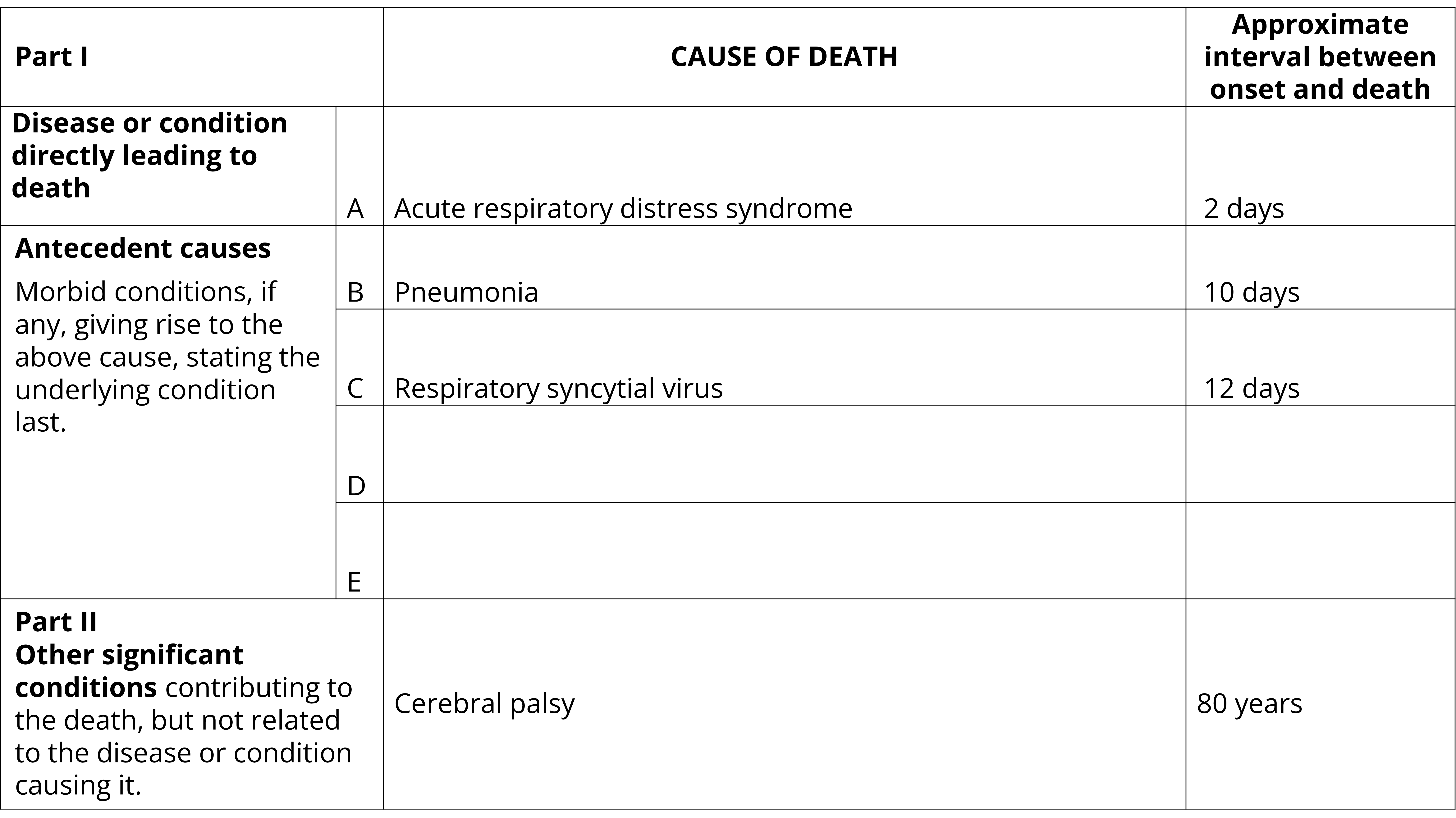
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Acute respiratory distress syndrome. Approximate interval between onset and death: 2 days
- Part 1(b): Pneumonia. Approximate interval between onset and death: 10 days
- Part 1(c): Respiratory syncytial virus. Approximate interval between onset and death: 12 days
- Parts 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Cerebral palsy. Approximate interval between onset and death: 80 years
Long COVID-19
If a past COVID-19 infection caused lasting complications which lead to death, the original infection should be certified on the MCCD. This is demonstrated in the following example.
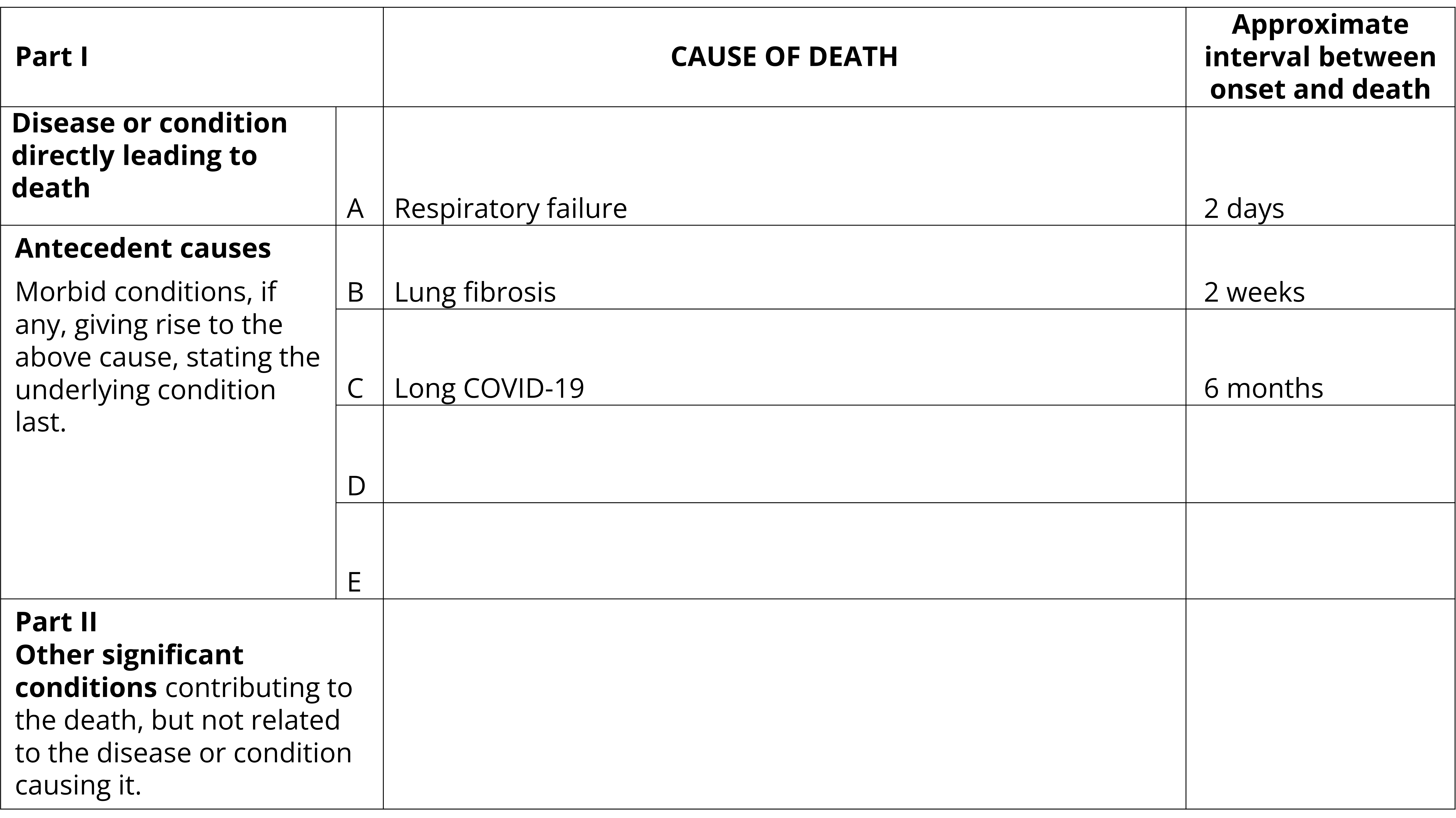
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Respiratory failure. Approximate interval between onset and death: 2 days
- Part 1(b): Lung fibrosis. Approximate interval between onset and death: 2 weeks
- Part 1(c): Long COVID-19. Approximate interval between onset and death: 6 months
- Parts 1(d), 1(e) and part 2: Blank. Approximate interval between onset and death: Blank
Acute respiratory infections as contributing causes of death
Acute respiratory infections should be recorded as a contributing cause of death where an individual is positive for a viral illness but there is a disease or injury pathway to death that is not directly caused by the virus. For example, a person may have late stage cancer that has metastasised extensively causing organ damage leading to death. This person may also have contracted COVID-19. While the virus or its complications may have negatively impacted health in an immuno-compromised person, the virus itself did not cause the terminal event leading to death (e.g. organ failure caused by metastases). In this circumstance, the viral illness should be certified in Part 2.
Incidental viral infections which did not contribute to the death should not be certified on the MCCD.
The following two examples show how an acute respiratory illness can be certified in Part 2 of the MCCD.
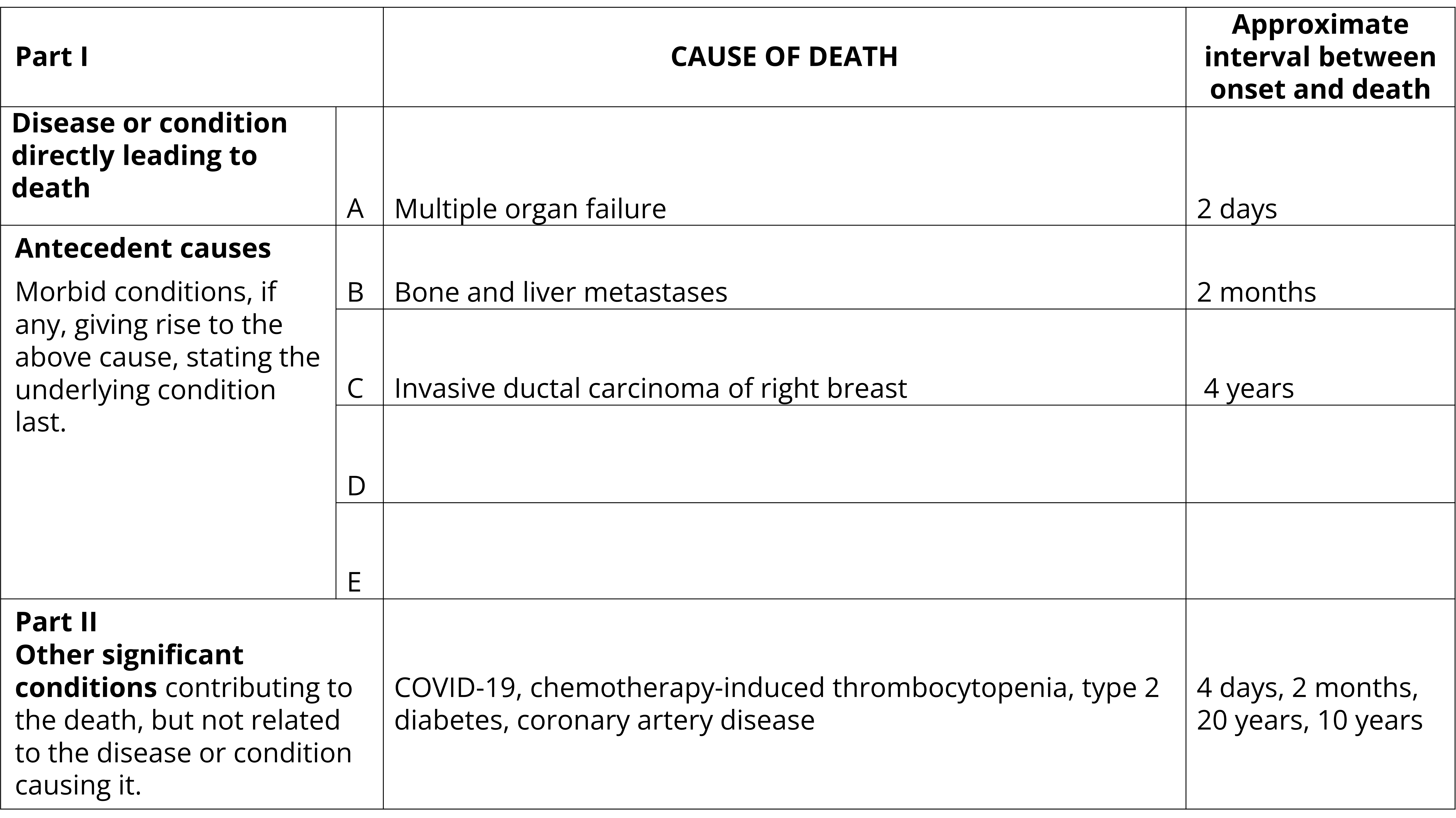
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Multiple organ failure. Approximate interval between onset and death: 2 days
- Part 1(b): Bone and liver metastases. Approximate interval between onset and death: 2 months
- Part 1(c): Invasive ductal carcinoma of right breast. Approximate interval between onset and death: 4 years
- Parts 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: COVID-19, chemotherapy-induced thrombocytopenia, type 2 diabetes, coronary artery disease. Approximate interval between onset and death: 4 days, 2 months, 20 years, 10 years
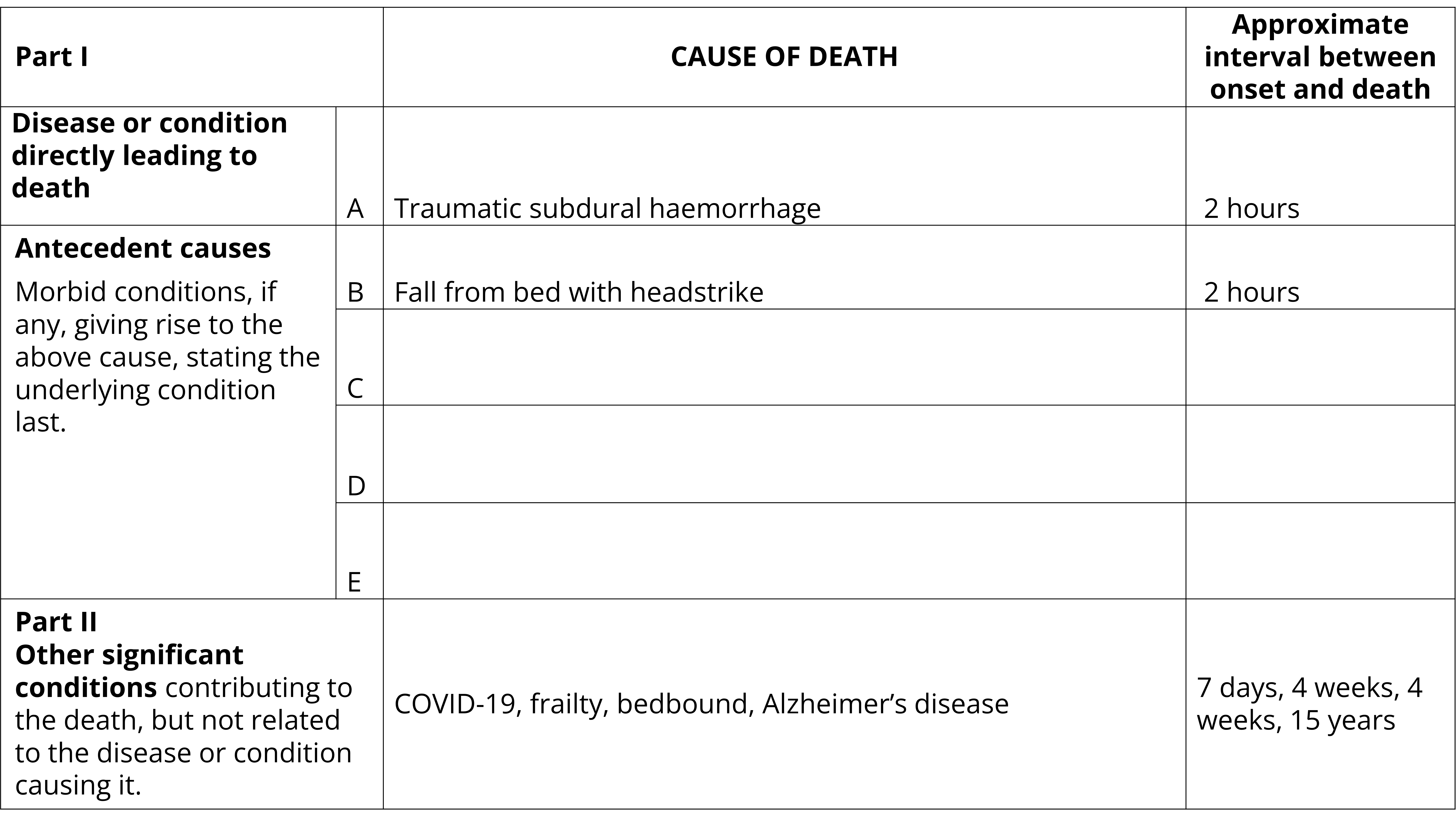
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Traumatic subdural haemorrhage. Approximate interval between onset and death: 2 hours
- Part 1(b): Fall from bed with headstrike. Approximate interval between onset and death: 2 hours
- Parts 1(c), 1(d) and 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: COVID-19, frailty, bedbound, Alzheimer’s disease. Approximate interval between onset and death: 7 days, 4 weeks, 4 weeks, 15 years
External causes
Injuries
Injuries should never be reported on the Medical Certificate of Cause of Death (MCCD) without the circumstances that led to the injury. In most instances, deaths occurring as the result of an accident must by law be referred to the coroner. When a medical practitioner has occasion to issue a MCCD relating to a death resulting from an accident, the circumstances of the accident as well as the injuries incurred need to be reported. For example, 'fractured skull with cerebral haemorrhage due to accidental fall on stairs at home' or 'fractured neck of femur due to fall from bed in nursing home'.
When certifying deaths due to external causes:
- Include all injuries sustained and avoid using non-specific terms such as 'multiple injuries'.
- If a death is due to late effects of a previous injury, state the circumstances of this injury, e.g. bronchopneumonia due to paraplegia due to motor vehicle accident 3 years ago.
- Always certify the reason for the injury (the mechanism of death).
- Check guidelines for referring a death to the coroner as most deaths due to external causes are reportable deaths in Australia.
The following example shows how a death due to an external cause may be certified. The manner (accident) and mechanism (trip on carpet) are clearly stated, as well as the resulting injury and associated complications. Risk factors which increased the propensity to fall and severity of the injury are also included in Part 2 of the certificate.
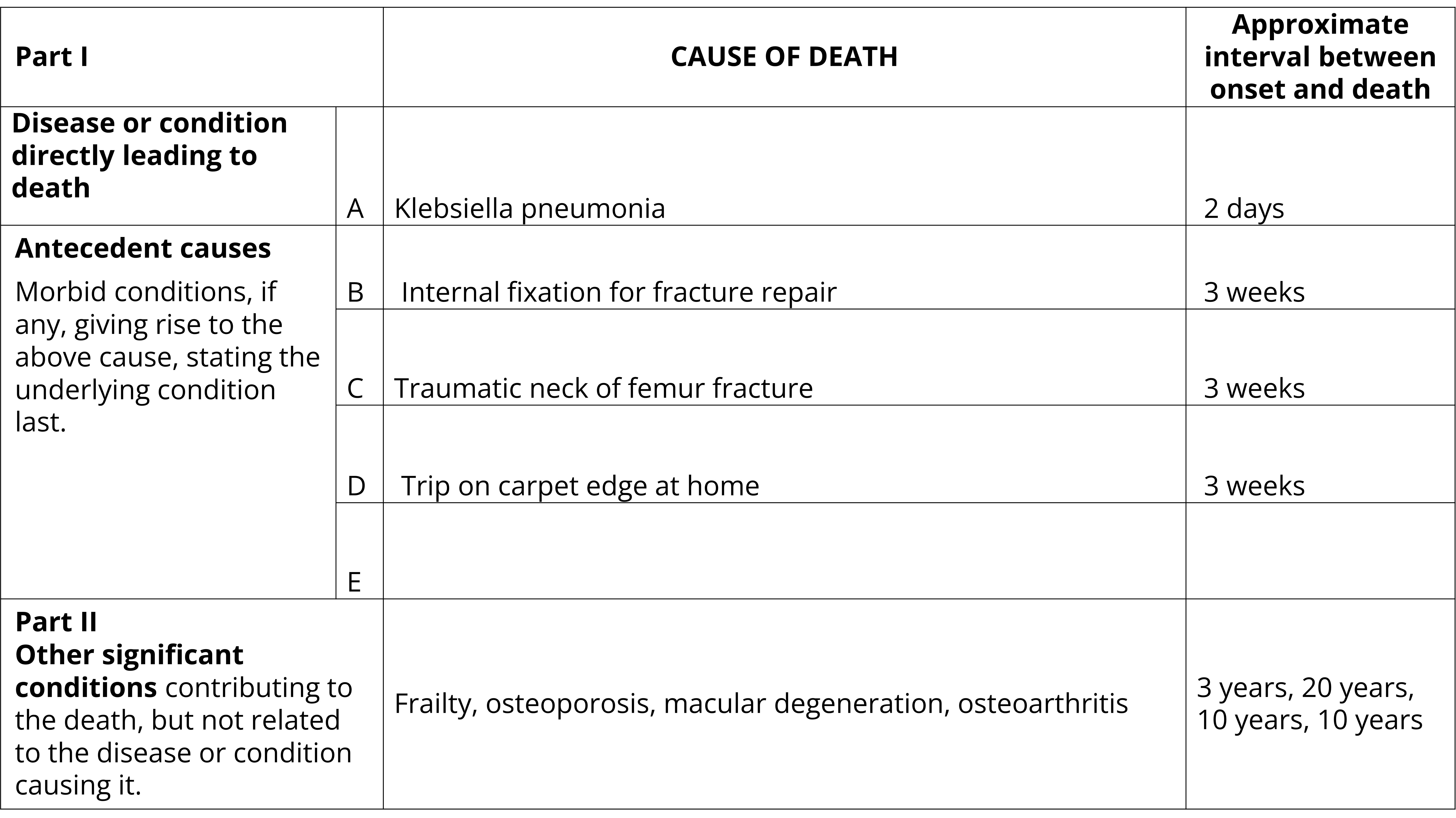
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Klebsiella pneumonia. Approximate interval between onset and death: 2 days
- Part 1(b): Internal fixation for fracture repair. Approximate interval between onset and death: 3 weeks
- Part 1(c): Traumatic neck of femur fracture. Approximate interval between onset and death: 3 weeks
- Part 1(d): Trip on carpet edge at home. Approximate interval between onset and death: 3 weeks
- Part 1(e): Blank
- Part 2: Frailty, osteoporosis, macular degeneration, osteoarthritis. Approximate interval between onset and death: 3 years, 20 years, 10 years, 10 years
Fractures
Certification of fractures
When certifying deaths due to fractures and other conditions for which the cause can be either traumatic or pathological, specify the nature and cause of the fracture. For traumatic fractures specify the mechanism or the cause of the injury (e.g. motor vehicle crash, fall down stairs) and the manner or intent of the injury (e.g. unintentional). For pathological fractures specify the disease or condition which resulted in the fracture (e.g. malignancy, osteoporosis).
The following example provides an example of how a traumatic fracture may be certified. The cause of the fracture is clearly clearly certified with the manner and mechanism indicating that it is a death due to trauma.
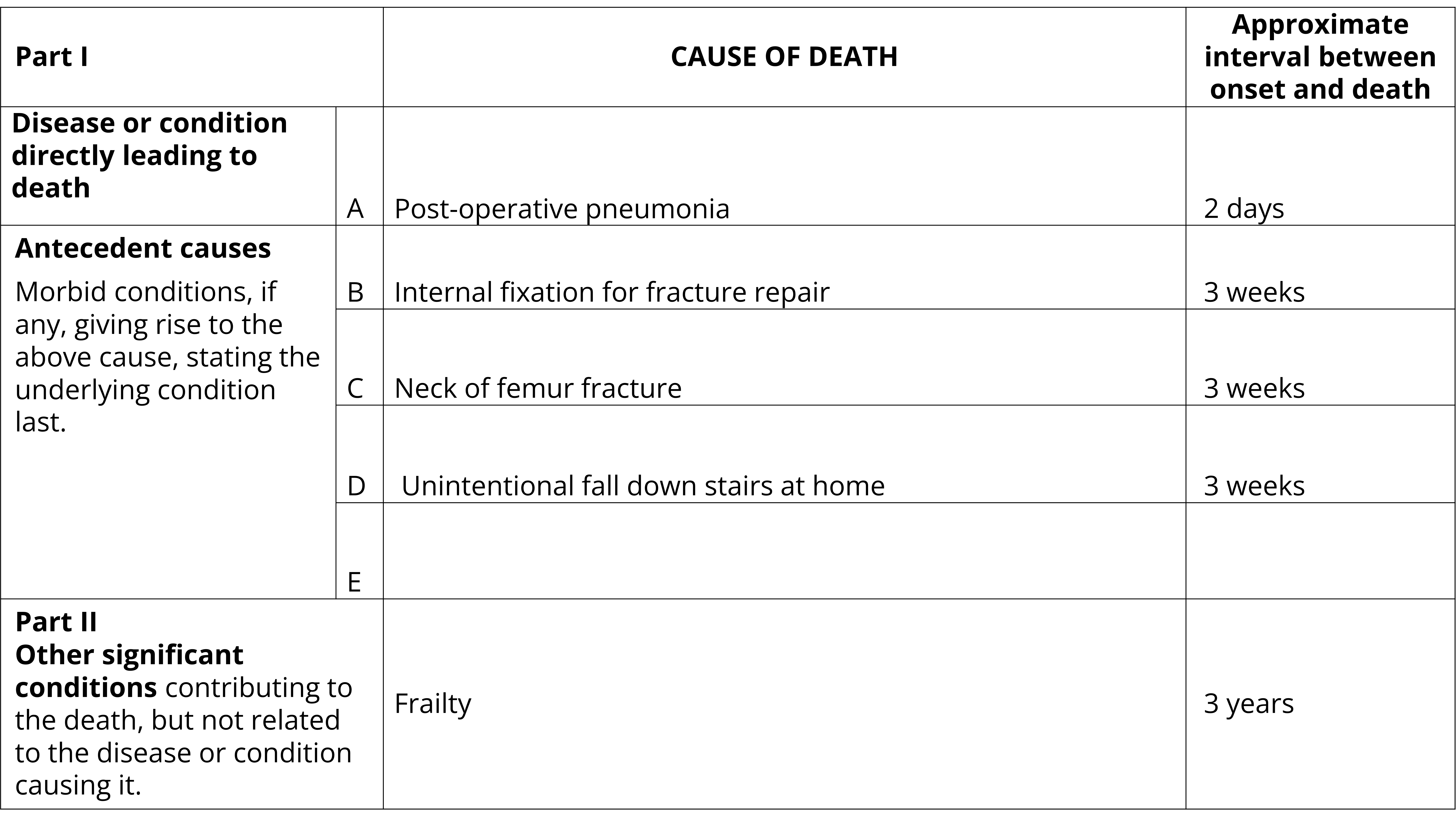
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Post-operative pneumonia. Approximate interval between onset and death: 2 days
- Part 1(b): Internal fixation for fracture repair. Approximate interval between onset and death: 3 weeks
- Part 1(c): Neck of femur fracture. Approximate interval between onset and death: 3 weeks
- Part 1(d): Unintentional fall down stairs at home. Approximate interval between onset and death: 3 weeks
- Part 1(e): Blank. Approximate interval between onset and death: Blank
- Part 2: Frailty. Approximate interval between onset and death: 3 years
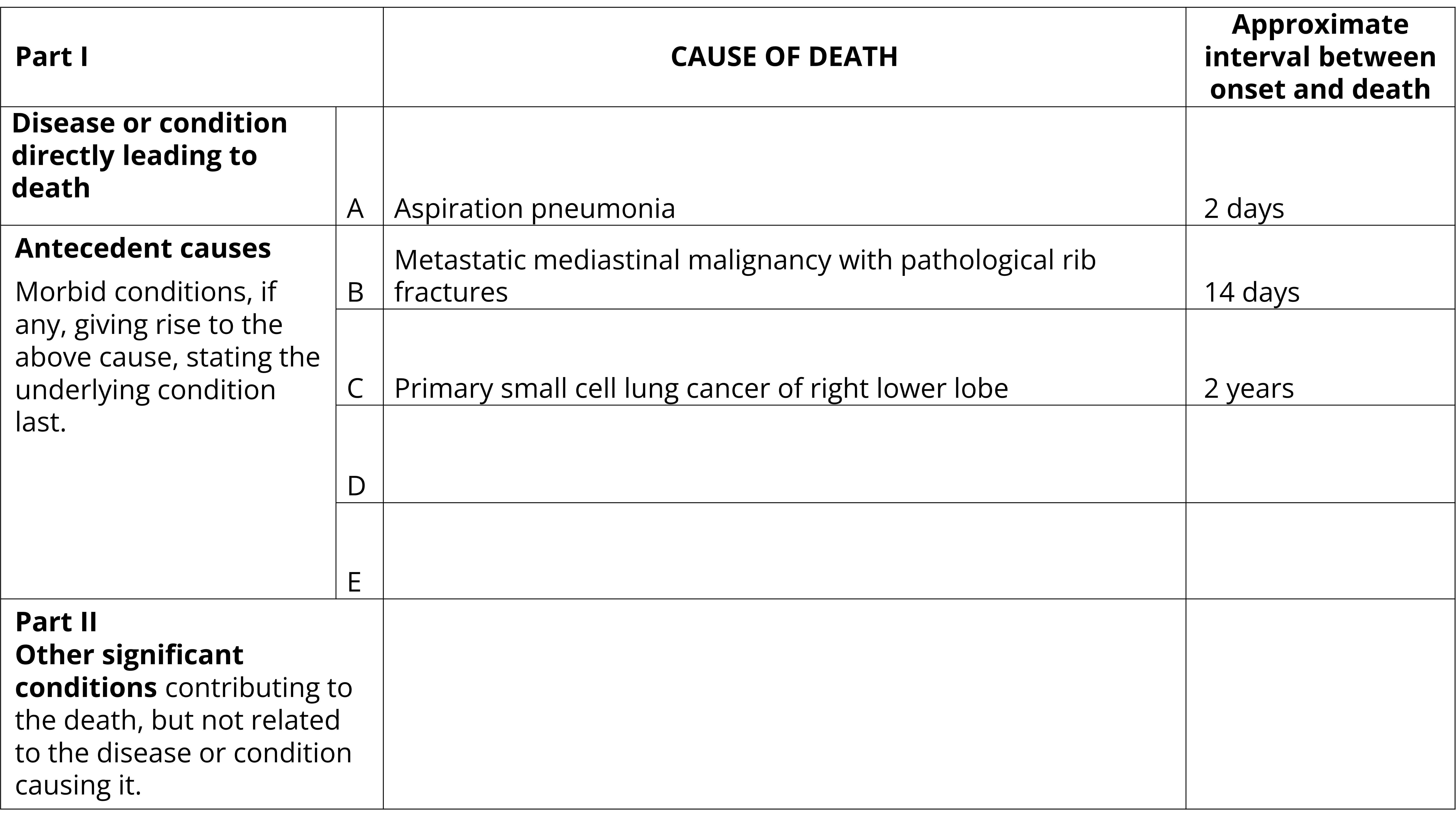
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Aspiration pneumonia. Approximate interval between onset and death: 2 days
- Part 1(b): Metastatic mediastinal malignancy with pathological rib fractures. Approximate interval between onset and death: 14 days
- Part 1(c): Primary small cell lung cancer of right lower lobe. Approximate interval between onset and death: 2 years
- Parts 1(d), 1(e) and 2: Blank. Approximate interval between onset and death: Blank
Skin conditions
Certification of skin conditions
When certifying conditions of the skin such as wounds, ulcers and haemorrhages specify whether the condition is traumatic or atraumatic. Specify the site, cause and any risk factors of the skin condition such as immobility, diabetes or vascular disease. Where applicable, specify if an infection is present and give the name of the causative organism where known. The following example demonstrates how a skin condition may be certified.
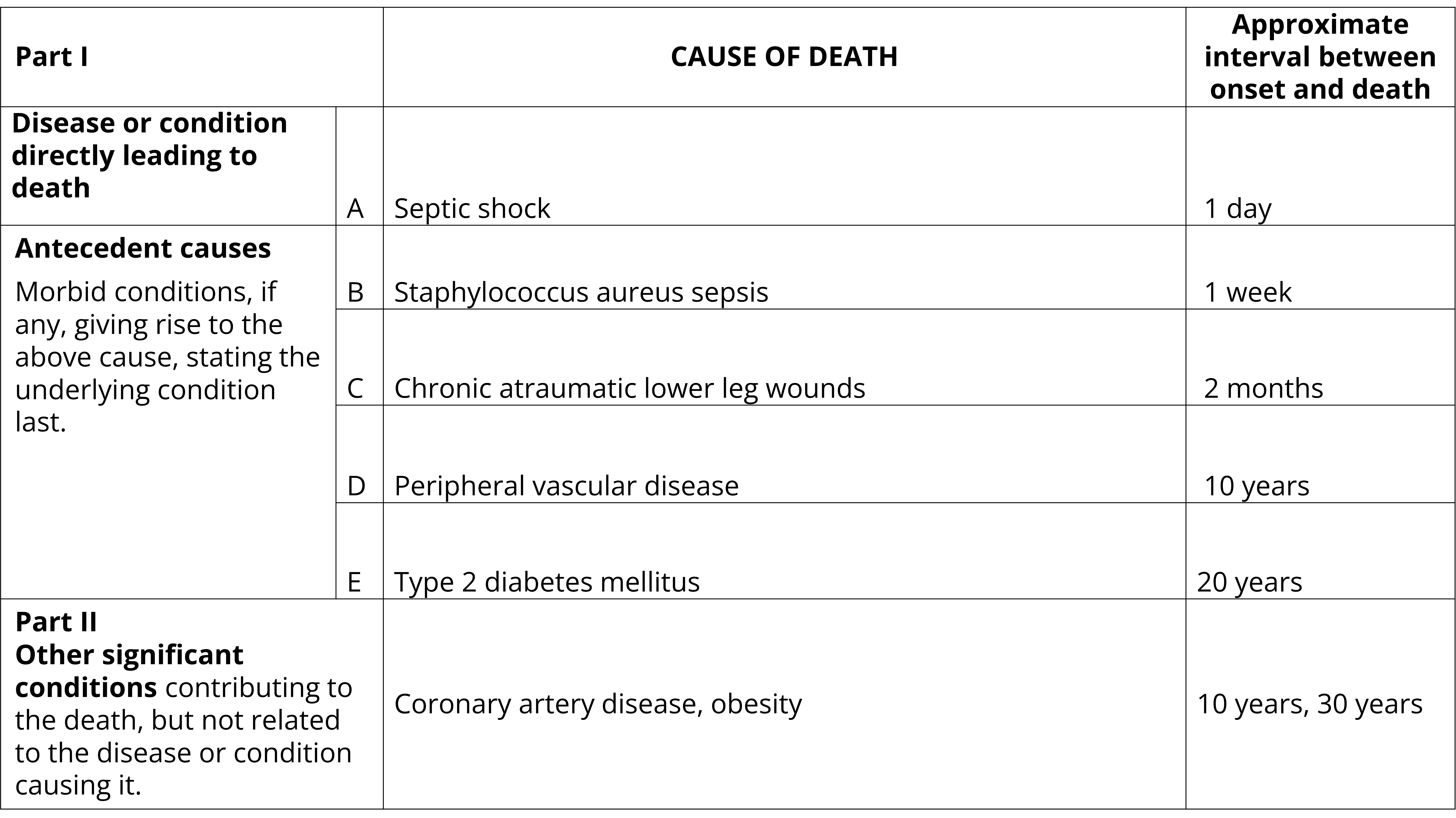
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Septic shock. Approximate interval between onset and death: 1 day
- Part 1(b): Staphylococcus aureus sepsis. Approximate interval between onset and death: 1 week
- Part 1(c): Chronic atraumatic lower leg wounds. Approximate interval between onset and death: 2 months
- Part 1(d): Peripheral vascular disease. Approximate interval between onset and death: 10 years
- Part 1(e): Type 2 diabetes mellitus. Approximate interval between onset and death: 20 years
- Part 2: Coronary artery disease, obesity. Approximate interval between onset and death: 10 years, 20 years
Rare conditions
Certification of rare conditions
It is accepted that on occasion a medical practitioner will have responsibility for certifying a death that is considered a rare occurrence in Australia. To ensure high quality data, the ABS reviews all records that are considered to be of a rare or improbable nature in Australia. To assist this process, it is important that when certifying deaths of this nature that additional information be provided on the certificate to confirm that condition has been proven histologically or through other extensive medical testing. As an example, if the disease that caused death is Creutzfeldt-Jakob Disease, then the addition of the term 'histologically proven' will ensure accurate code assignment. The list below, whilst not exhaustive, provides examples of the types of conditions that are considered to be rare or impossible in Australia.
- Acute poliomyelitis
- Anthrax
- Botulism
- Creutzfeldt-Jakob Disease
- Diphtheria
- Q fever
- Rabies
- Smallpox
- Typhoid fever
- Yellow fever
The following example shows how a death due to a rare disease may be certified.
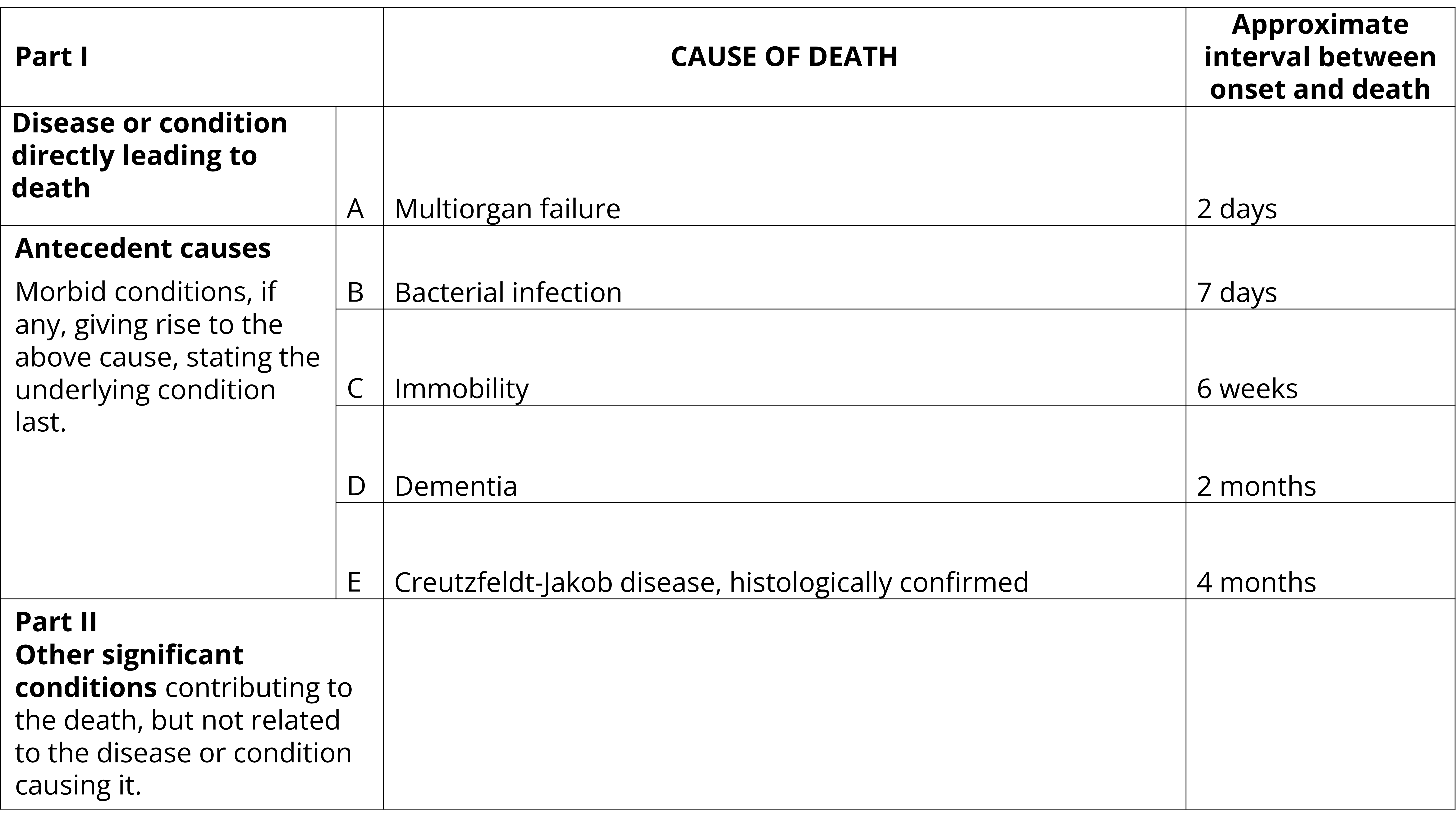
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line. The certificate is filled out as follows:
- Part 1(a): Multiorgan failure. Approximate interval between onset and death: 2 days
- Part 1(b): Bacterial infection. Approximate interval between onset and death: 7 days
- Part 1(c): Immobility. Approximate interval between onset and death: 6 weeks
- Part 1(d): Dementia. Approximate interval between onset and death: 2 months
- Part 1(e): Creutzfeldt-Jakob disease, histologically confirmed. Approximate interval between onset and death: 4 months
- Part 2: Blank. Approximate interval between onset and death: Blank
Pulmonary embolism
Certification of pulmonary embolism
It is rare for a pulmonary embolism to occur spontaneously in anyone below 75 years of age and there are a large variety of underlying causes of this condition. Where pulmonary embolism is the direct cause or mode of death it should be entered as such in Line 1(a) of the death certificate, with its underlying cause(s) sequenced in the ‘due to’ relationship on the lines below it. This is demonstrated in the following example.
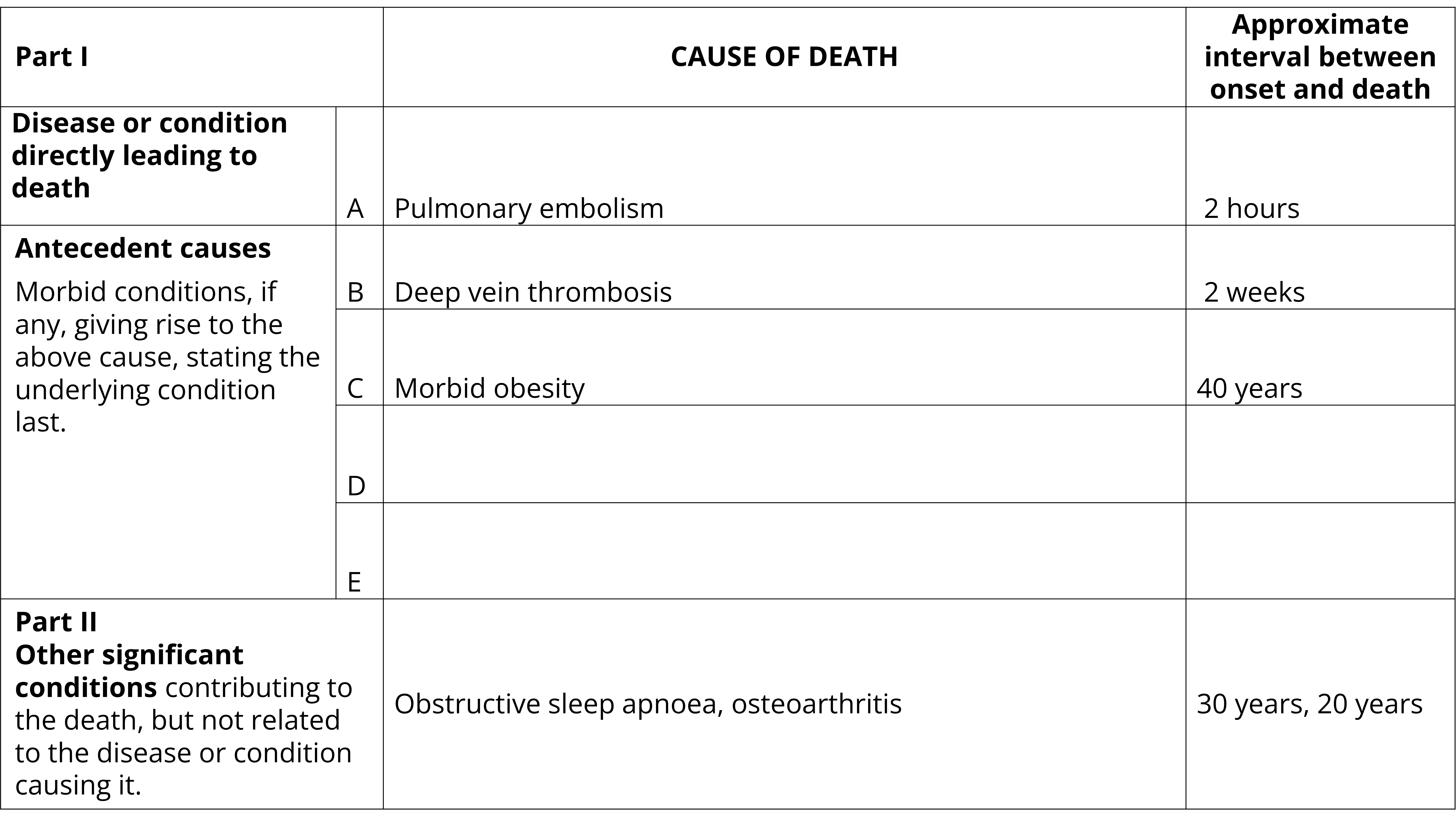
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): Pulmonary embolism. Approximate interval between onset and death: 2 hours
- Part 1(b): Deep vein thrombosis. Approximate interval between onset and death: 2 weeks
- Part 1(c): Morbid obesity. Approximate interval between onset and death: 40 years
- Part 1(d): Blank. Approximate interval between onset and death: Blank
- Part 2: Obstructive sleep apnoea, osteoarthritis. Approximate interval between onset and death: 30 years, 20 years
Renal failure
Certification of renal failure
Where renal failure is entered on the Medical Certificate of Cause of Death, identify:
- If the renal failure was acute, chronic or end-stage. If known, put the stage of kidney disease (e.g. chronic kidney disease stage 4).
- The cause of the renal failure if known.
The following example shows how renal failure may be certified on the MCCD. The cause of the renal failure is clearly certified.
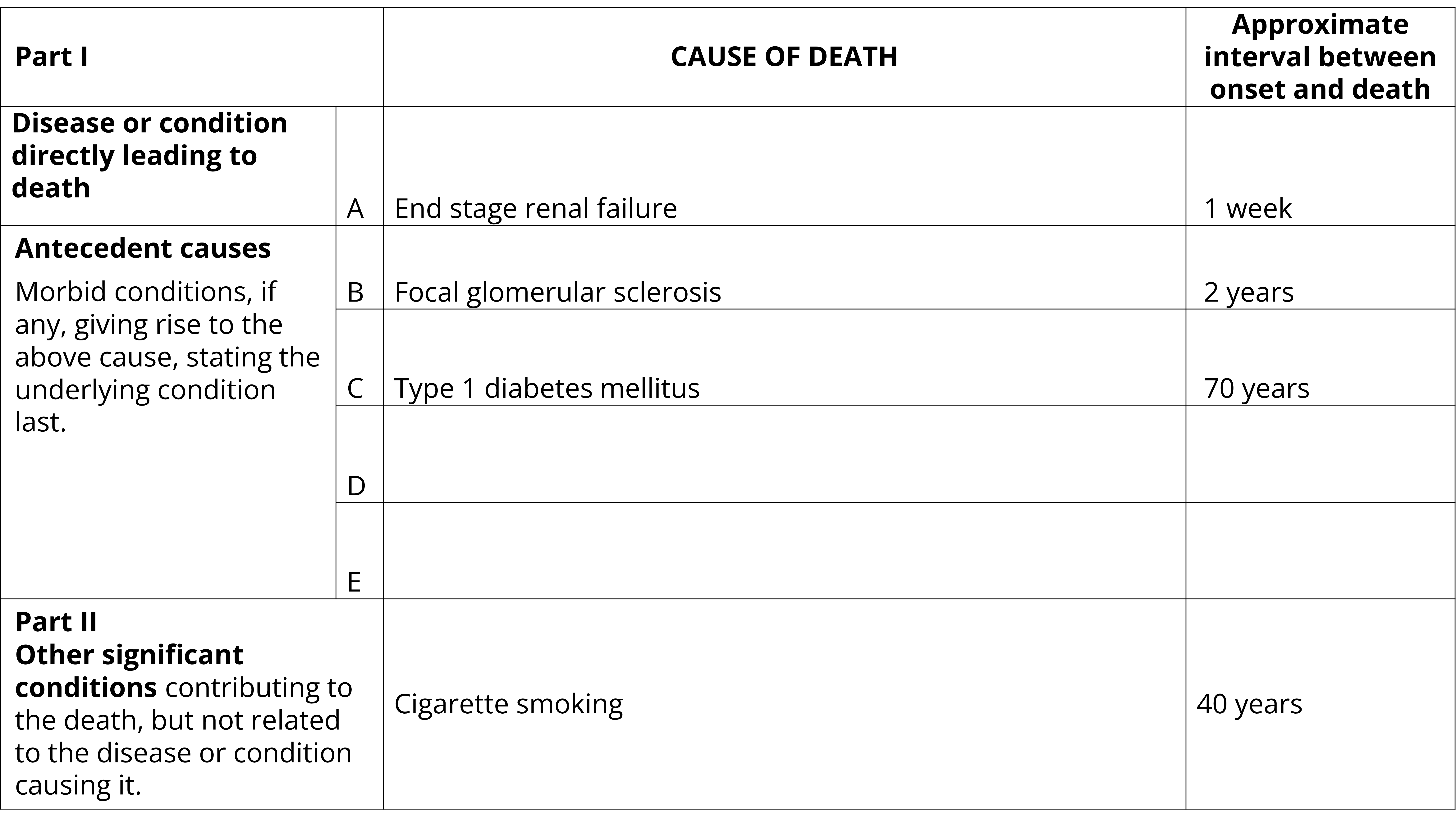
Example of a completed Medical Certificate of Cause of Death. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1(a): End stage renal failure. Approximate interval between onset and death: 1 week
- Part 1(b): Focal glomerular sclerosis. Approximate interval between onset and death: 2 years
- Part 1(c): Type 1 diabetes mellitus. Approximate interval between onset and death: 70 years
- Part 1(d): Blank. Approximate interval between onset and death: Blank
- Part 2: Cigarette smoking. Approximate interval between onset and death: 40 years
Perinatal deaths
Medical Certificate of Cause of Perinatal Death
A perinatal death is a death that is either a:
- fetal death (i.e. a death prior to the complete expulsion or extraction from its mother as a product of conception)
- neonatal death (i.e. death of a live born baby within 28 completed days of birth).
For most jurisdictions, a perinatal death is certified using a Medical Certificate of Cause of Perinatal Death (MCCPD). The exception is Tasmania where the Medical Certificate of Cause of Death is used for certifying both general deaths and perinatal deaths. The MCCPD varies across jurisdictions. Information on the MCCPD used in each jurisdiction is detailed below.
In alignment with the World Health Organization and the International Classification of Diseases used by the ABS for coding of causes of death information, the American spelling of the word 'fetus' has been used throughout this guide. This spelling may vary to that used on the MCCPD by some jurisdictions where 'foetus' may be used.
New South Wales, Queensland, Northern Territory and Australian Capital Territory
The MCCPD used in New South Wales, Queensland, the Northern Territory and the Australian Capital Territory seeks information on maternal obstetric history with a view to identifying those conditions which require the greatest clinical monitoring to avoid the occurrence of perinatal deaths. The process of recording a sequence of events leading to the death is not used for the MCCPD in these jurisdictions.
The MCCPD provides five lines for the entry of causes of perinatal deaths. In Line (a) and Line (b) enter the diseases or conditions of the infant or fetus. The single most important or main condition in the infant or fetus should be entered in Line (a) and the remainder, if any, in Line (b). The 'most important' or 'main condition' is the pathological condition which, in the opinion of the certifier made the greatest contribution to the death of the infant or fetus. The mode of death, eg. heart failure, asphyxia, anoxia, should not be entered in Line (a) unless it was the only fetal or infant condition known.
In Line (c) and Line (d), the certifier should enter all diseases or conditions in the mother which contributed to the death of the infant or fetus. The maternal condition considered the most contributory of these should be entered in Line (c) and the others, if any, in Line (d).
Line (e) (labelled 'Part 2' in Queensland) is provided for the reporting of any other circumstances considered to have had a bearing on the death, but which cannot be described as a disease or condition of the infant or the mother. Examples of this might be delivery in the absence of a birth attendant or involvement in a motor vehicle accident.
The following example shows how a perinatal death may be certified in New South Wales, Queensland, the Northern Territory and the Australian Capital Territory.
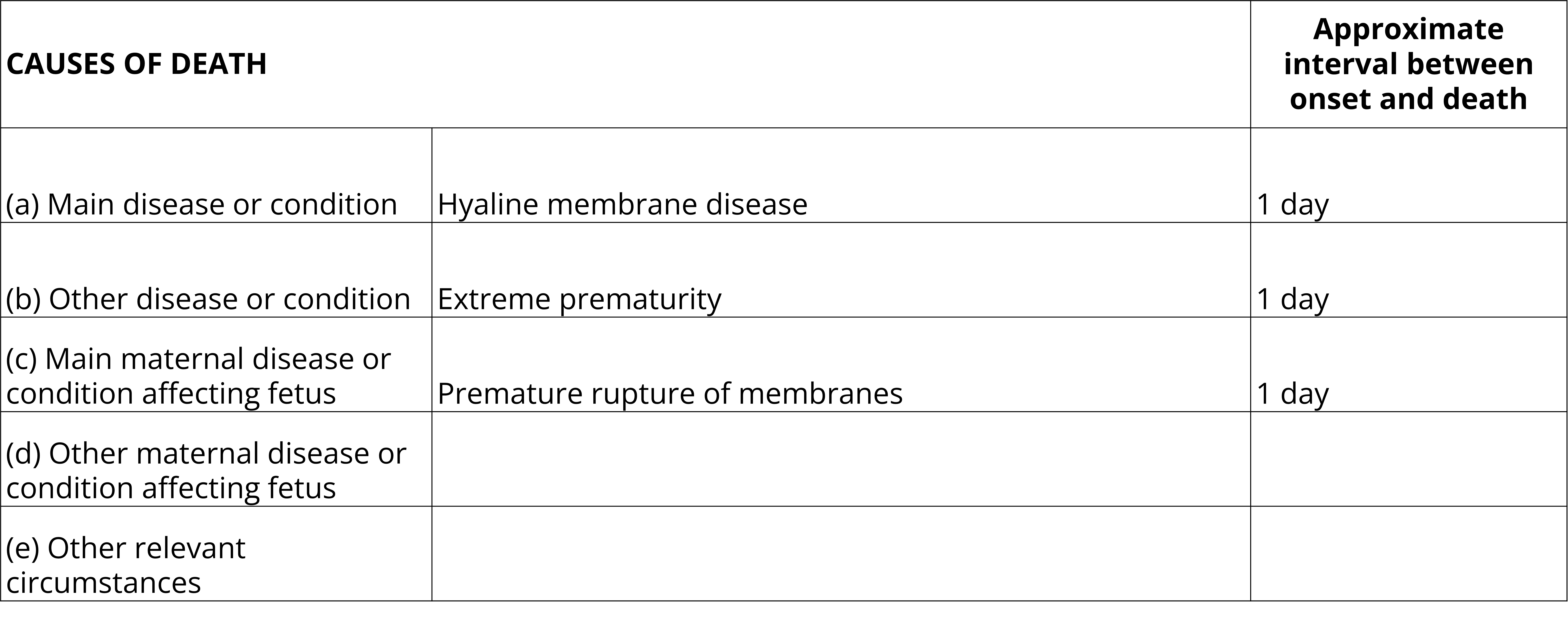
Example of a completed Medical Certificate of Cause of Perinatal Death used in New South Wales, Queensland, Northern Territory and Australian Capital Territory. The certificate contains 5 lines for completion. Line (a) for the main disease or condition, Line (b) for other disease or condition, Line (c) for the main maternal disease or condition affecting fetus, Line (d) for other maternal disease or condition affecting fetus and Line (e) for other relevant circumstances. There is also a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Line (a): Hyaline membrane disease. Approximate interval between onset and death: 1 day
- Line (b): Extreme prematurity. Approximate interval between onset and death: 1 day
- Line (c): Premature rupture of membranes. Approximate interval between onset and death: 1 day
- Lines (d) and (e): Blank.
South Australia
The MCCPD used in South Australia seeks information on maternal obstetric history, with a view to identifying those conditions which require the greatest clinical monitoring to avoid the occurrence of perinatal deaths. The process of recording a sequence of events leading to the death is not used for the MCCPD in South Australia.
The MCCPD provides five lines for the entry of causes of perinatal deaths. In Line (1) and Line (2) enter the diseases or conditions of the infant or fetus. The single most important or main condition in the child should be entered in Line (1) and the remainder, if any, in Line (2). The 'most important' or 'main condition' is the pathological condition which, in the opinion of the certifier made the greatest contribution to the death of the infant or fetus. The mode of death, eg. heart failure, asphyxia, anoxia, should not be entered in Line (1) unless it was the only fetal or infant condition known.
In Line (3) and Line (4), the certifier should enter all diseases or conditions in the mother which contributed to the death of the fetus. The maternal condition considered the most contributory of these should be entered in Line (3) and the others, if any, in Line (4).
Line (5) is provided for the reporting of any other circumstances which the certifier considers to have a bearing on the death, but which cannot be described as a disease or condition of the infant or the mother. Examples of this might be delivery in the absence of an attendant or involvement in a motor vehicle accident.
The following example shows how a perinatal death may be certified on the MCCPD in South Australia.
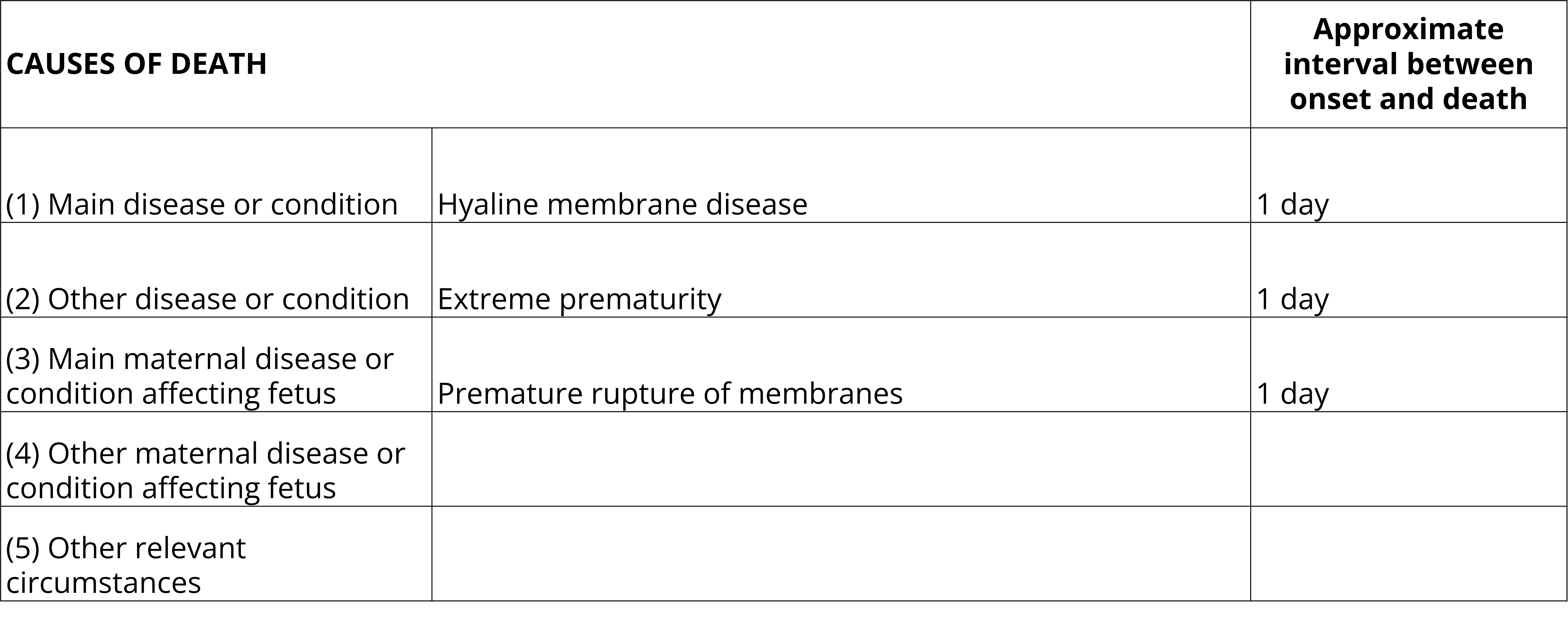
Example of a completed Medical Certificate of Cause of Perinatal Death used in South Australia. The certificate contains 5 lines for completion. Line (1) for the main disease or condition, Line (2) for other disease or condition, Line (3) for the main maternal disease or condition affecting fetus, Line (4) for other maternal disease or condition affecting the fetus and Line (5) for other relevant circumstances. There is also a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Line (1): Hyaline membrane disease. Approximate interval between onset and death: 1 day
- Line (2): Extreme prematurity. Approximate interval between onset and death: 1 day
- Line (3): Premature rupture of membranes. Approximate interval between onset and death: 1 day
- Lines (4) and (5): Blank.
Victoria
The MCCPD used in Victoria seeks information on the sequence of conditions in the child or fetus leading to the death. It also requires information on maternal conditions with a view to identifying those conditions which require the greatest clinical monitoring to avoid the occurrence of perinatal deaths.
In Part (A) enter the diseases or conditions of the infant or fetus. On Line (a) enter the disease or condition in the infant or fetus directly leading to death. If the direct cause of death as described in Line (a) was due to, or arose as a consequence of another disease, injury or condition, this should be reported in Line (b). Similarly, if the condition reported on Line (b) was due to another condition, report this on Line (c).
In Part (B), the certifier should enter all diseases or conditions in the mother giving rise to the underlying cause of death of the child or fetus.
There is also a section provided for details of any other significant condition(s) of the child, fetus or mother contributing to the death but not related to the disease, injury or condition causing it.
The following example shows how a perinatal death may be certified on the MCCPD in Victoria.
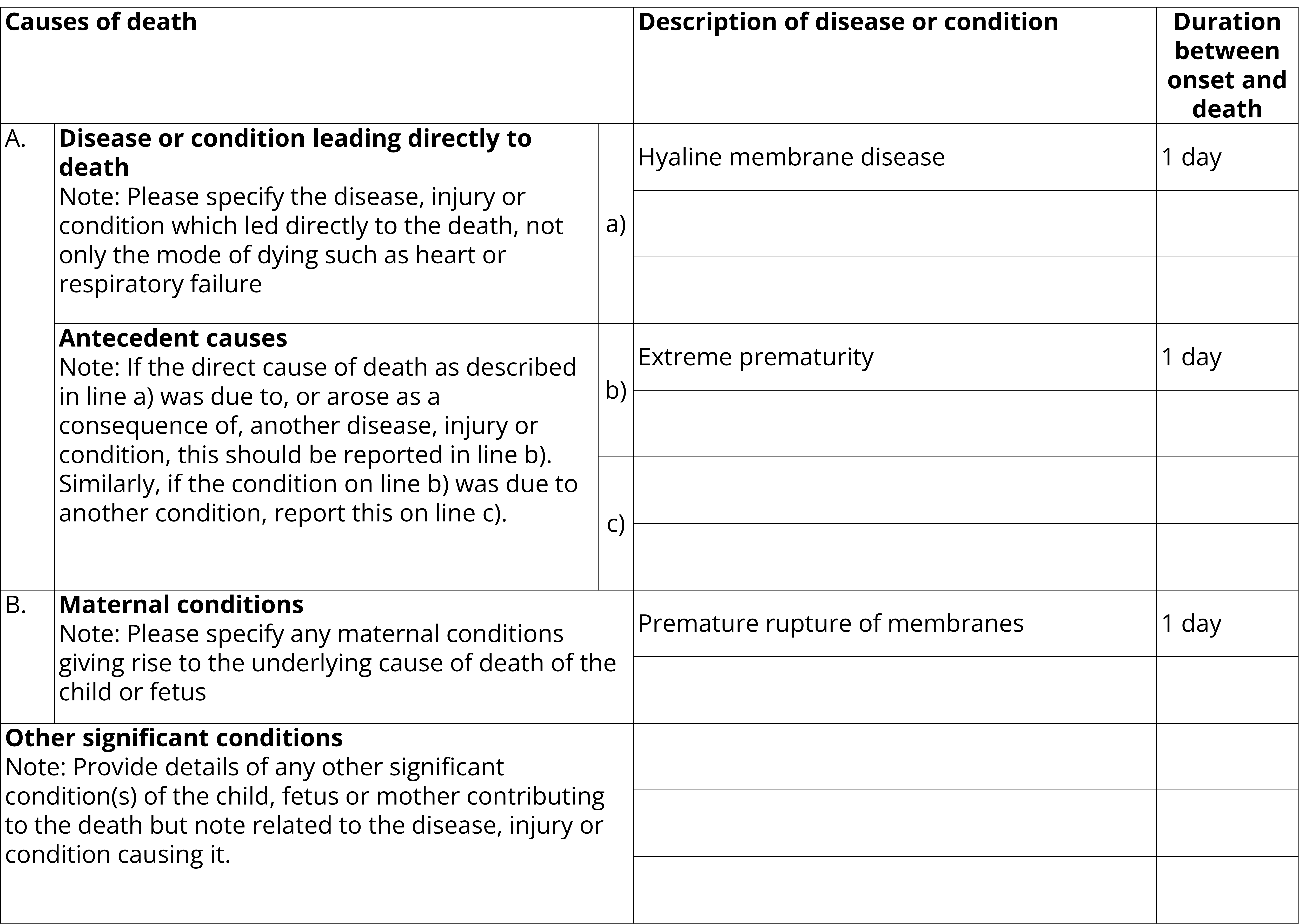
Example of a completed Medical Certificate of Cause of Perinatal Death used in Victoria. The certificate contains a Part A: Line (a) for the disease or condition leading directly to death, and Line (b) and Line (c) for antecedent causes. It also contains a Part B for maternal conditions and an additional section for other significant conditions. There is also a column to record the duration between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part A, Line (a): Hyaline membrane disease. Approximate interval between onset and death: 1 day
- Part A, Line (b): Extreme prematurity. Approximate interval between onset and death: 1 day
- Part A, Line (c): Blank. Approximate interval between onset and death: 1 day
- Part B: Premature rupture of membranes. Approximate interval between onset and death: 1 day
- Other significant conditions: Blank.
Western Australia
The MCCPD used in Western Australia seeks information on the sequence of conditions in the child or fetus leading to the death. It also requires information on maternal conditions with a view to identifying those conditions which require the greatest clinical monitoring to avoid the occurrence of perinatal deaths.
The MCCPD provides six lines for the entry of causes of perinatal deaths. On Line (a) enter the disease or condition in the infant or fetus leading directly to death. If this direct cause of death as described in Line (a) was due to, or arose as a consequence of another disease, injury or condition, this should be reported in Line (b). Similarly, if the condition reported on Line (b) was due to another condition, report this on Line (c).
On Line (d), the certifier should enter any maternal or other conditions or causes giving rise to the underlying cause of death of the child or fetus. If this maternal or other condition described in Line (d) was due to, or arose as a consequence of another disease, injury or condition, this should be reported in Line (e).
There is also a section to provide details of any other significant condition(s) of the child, fetus or mother contributing to the death but not related to the disease, injury or condition causing it.
The following example shows how a perinatal death may be certified in Western Australia.
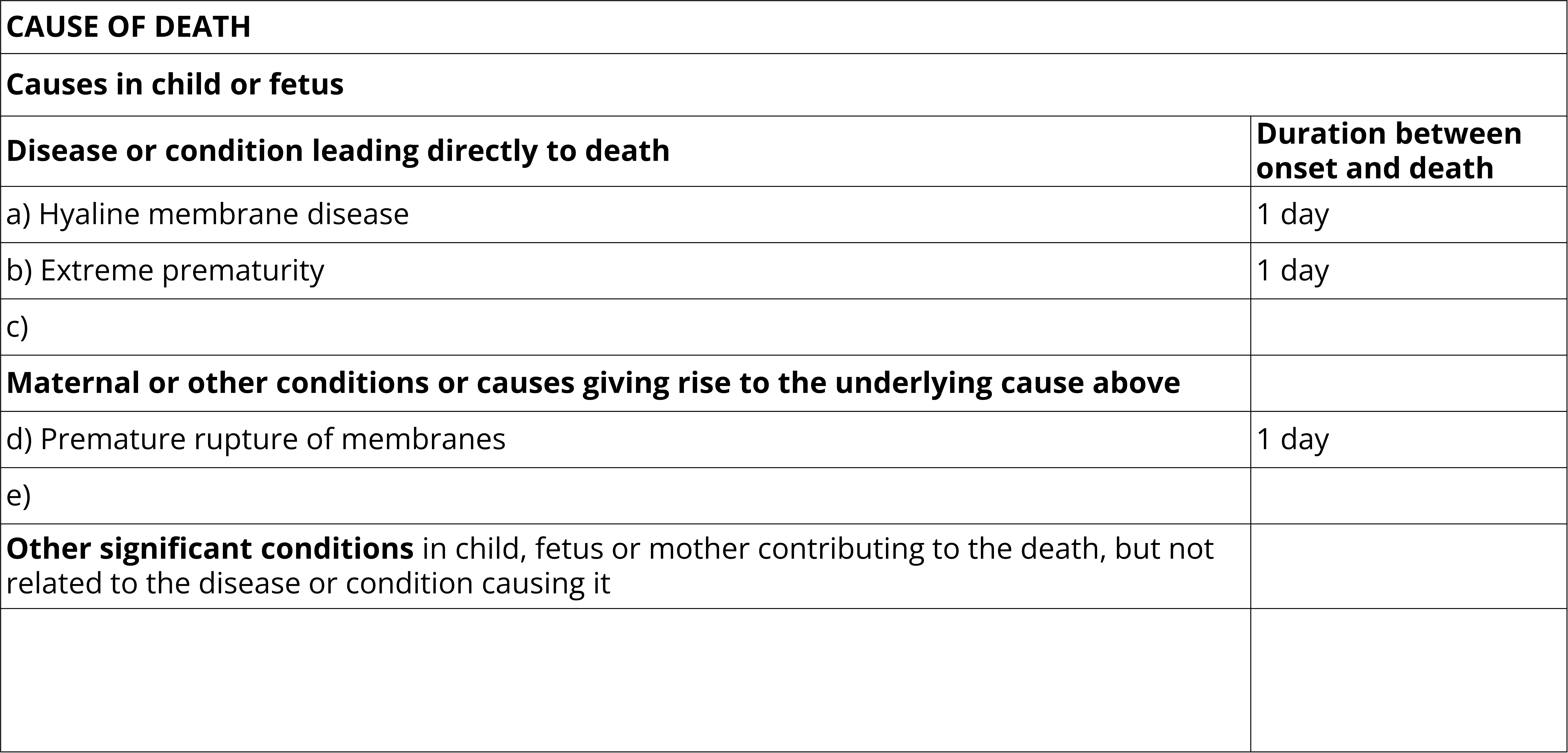
Example of a completed Medical Certificate of Cause of Perinatal Death used in Western Australia. The certificate contains 6 lines for completion. Lines (a), (b) and (c) are for the disease or condition leading directly to death. Lines (d) and (e) are for maternal or other conditions giving rise to the underlying cause above. There is a final line for other significant conditions. There is also a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Line (a): Hyaline membrane disease. Approximate interval between onset and death: 1 day
- Line (b): Extreme prematurity. Approximate interval between onset and death: 1 day
- Line (c): Blank
- Line (d): Premature rupture of membranes. Approximate interval between onset and death: 1 day
- Line (e): Blank
- Other significant conditions: Blank
Tasmania
In Tasmania, perinatal deaths should be certified utilising the same MCCD and certification guidelines as for general deaths. The following example shows how a perinatal death may be certified in Tasmania.
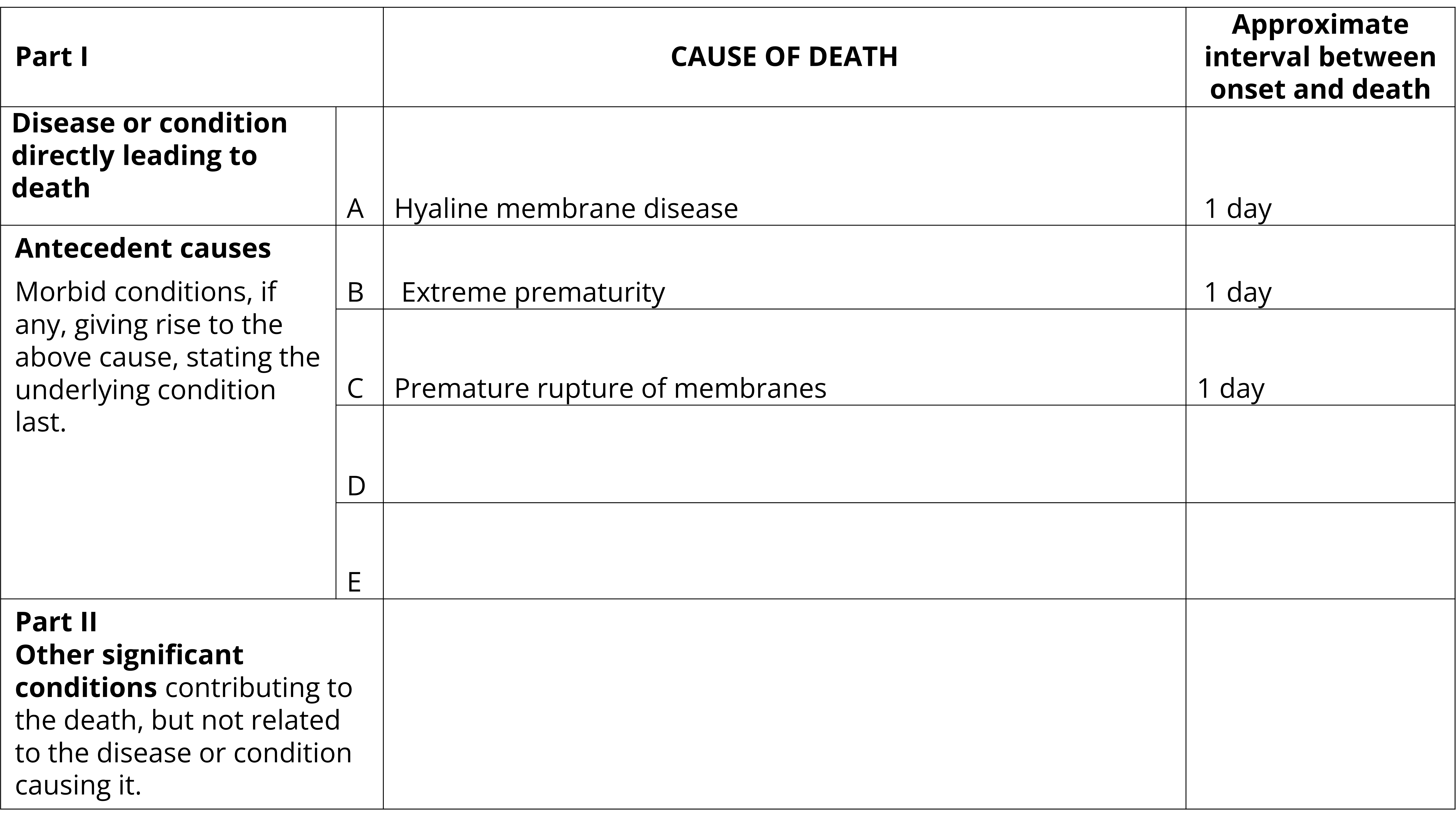
Example of a completed Medical Certificate of Cause of Perinatal Death used in Tasmania. The certificate contains 6 lines for completion separated into two parts. Part 1, line A for the disease or condition leading directly to death. Part 1 lines B, C, D and E for antecedent causes which are morbid conditions, if any, giving rise to the above cause, stating the underlying condition last. Part 2 of the certificate is a single line for other significant conditions contributing to the death but not directly related to the disease or condition causing it. For both Part 1 and Part 2 there is a column to record the approximate interval between onset and death for the conditions on each line.
The certificate is filled out as follows:
- Part 1 (A): Hyaline membrane disease. Approximate interval between onset and death: 1 day
- Part 1 (B): Extreme prematurity. Approximate interval between onset and death: 1 day
- Part 1 (C): Premature rupture of membranes. Approximate interval between onset and death: 1 day
- Parts 1(D), 1(E) and 2: Blank
Common certification issues
Congenital malformations
Specify the organ and part of organ involved, unless this is obvious from the name of the malformation. Specify that the condition was ‘congenital’ as opposed to ‘acquired’ where applicable. Avoid the use of eponyms wherever possible.
Birth injuries
Clearly state the organ involved, the type of injury (e.g. haemorrhage, tear) and the cause of the injury (e.g. abnormality of pelvis, malposition of fetus, abnormal forces of labour).
Conditions in the mother
Indicate whether any disease or condition present in the mother was related to the pregnancy. For example, conditions such as hypertension and pyelonephritis should be qualified as to whether they arose during pregnancy or were present before pregnancy.
Prematurity and premature labour
Prematurity and premature labour are not detailed enough to be assigned as an underlying cause of perinatal death. If the cause of the premature labour is known, specify this on the certificate. For example, premature labour due to membrane rupture.
Specificity
Specify where conditions are congenital versus acquired. For conditions that can materialise in both the mother and/or the baby, specify whether the condition is occurring in the mother or baby.