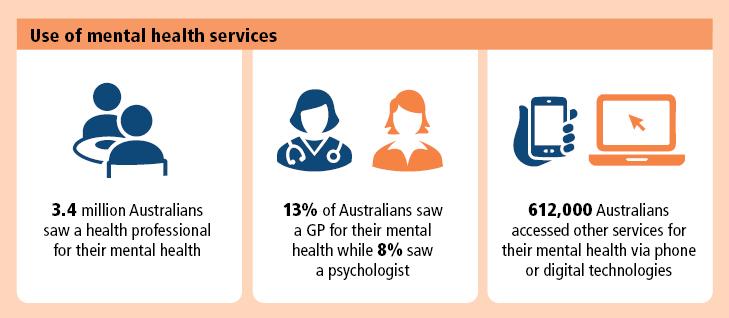
Consultations with health professionals for mental health
Respondents were asked about consultations with health professionals for mental health in the 12 months prior to interview. These included:
- general practitioner
- psychiatrist
- psychologist
- mental health nurse
- other mental health professional – e.g. social worker, counsellor, occupational therapist
- specialist doctor or surgeon – e.g. cardiologist, gynaecologist or urologist
- other health professional – e.g. dietician, physiotherapist, pharmacist (advice only).
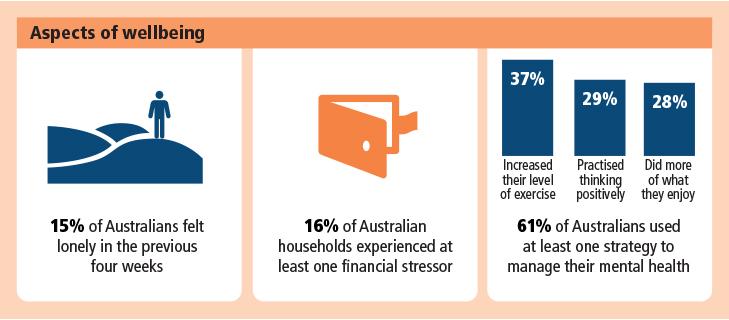
Financial stress
One person in the household was asked to report on behalf of the entire household whether they experienced one or more of the following due to a shortage of money in the 12 months prior to interview:
- pawned or sold something because of a shortage of money
- went without meals
- went without dental treatment when needed
- were unable to heat or cool your home
- sought financial assistance from friends or family
- sought assistance from welfare or community organisations
- could not pay electricity, gas or telephone bills on time
- could not pay mortgage or rent payments on time
- could not pay for car registration or insurance on time
- could not pay home and/or contents insurance on time
- could not make minimum payment on credit card.
Household
One or more persons usually resident in the same private dwelling.
Loneliness
Respondents were asked whether they felt lonely in the last 4 weeks prior to interview. This question was asked as part of a selected group of questions from the Living in the Community Questionnaire - Summary (LCQ-S). The LCQ-S was developed by the Australian Mental Health Outcomes and Classification Network (AMHOCN) to assess social support and societal participation of Australians.
Other services for mental health accessed using digital technologies
In addition to consultations with health professionals for mental health, respondents were asked whether they had accessed other services for their mental health using digital technologies, including the phone or internet in the 12 months prior to interview. Types of services included:
- crisis support or counselling services
- treatment programs, training, assessment or other tools to improve mental health
- mental health support groups, forums or chat rooms.
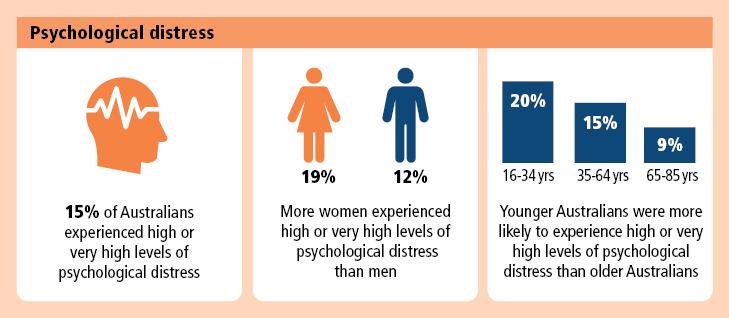
Psychological distress
The study collected information on psychological distress using the Kessler Psychological Distress Scale (K10). The Kessler Psychological Distress Scale (K10) is a widely used indicator, which gives a simple measure of psychological distress.
Respondents were asked how often in the last four weeks they had felt:
- tired out for no good reason
- nervous
- so nervous that nothing could calm you down
- hopeless
- restless or fidgety
- so restless you could not sit still
- depressed
- everything was an effort
- so sad that nothing could cheer you up
- worthless.
Using these questions, a five-level response scale that corresponded to scores from 1 for ‘none of the time’ to 5 for ‘all the time’ were summed, with low scores indicating low levels of psychological distress and high scores indicating high levels of psychological distress.
Results are grouped according to the following categories:
- low (scores of 10-15, indicating little or no psychological distress)
- moderate (scores of 16-21)
- high (scores of 22-29)
- very high (scores of 30-50).
Self-management strategies for mental health
Respondents were asked about self-management strategies they used for their mental health in the last 12 months. These included:
- taken non-prescription medicines, vitamins, supplements or herbal remedies
- changed your diet
- practised meditation, mindfulness, yoga or other relaxation techniques
- better organised home, life and other things
- practised thinking positively and setting achievable goals
- increased your level of exercise or physical activity
- done more of the things you enjoy
- seek support from family or friends
- used alcohol or drugs
- cut out alcohol or drugs
- other.